India with the highest TB burden globally has made a drastic shift recently to reach the unreached people with free TB services. Indian government has launched a 100 days focussed campaign (7 December 2024 to 24 March 2025) to intensify progress to #endTB through improved case detection, reduction in diagnostic delays, and enhanced treatment outcomes across 347 most affected districts in 33 states of the country.
The aim is to find the missing TB cases in the most at risk communities – as early as possible – to help stop further spread of infection and reduce unnecessary human suffering and risk of TB death (by putting those diagnosed with TB on an effective treatment, and those with latent TB on TB preventive therapy).
India’s Health Minister Sri Jagat Prakash Nadda had said two weeks ago that the “focussed campaign of 100 Days is an effort to quickly detect and treat TB patients in 347 most affected districts in 33 states across the country. The government is working on the 4Ts – Test, Track, Treat and Technology – to eliminate TB.”
These 347 districts of India (out of around 800 districts in the country) were chosen on the basis of- if TB mortality rate in 2023 was equal to or more than the national average of 3.6%, or the identification of new and potential TB cases was below the national average of 1700 per 100,000 population, or TB incidence rate was equal to more than 200 per 100,000 population, or TB prevalence rate was over 400 per 100,000 population. Maximum number of the districts are in the southern state of Karnataka (31), followed closely by Maharashtra (30), among other states or union territories.
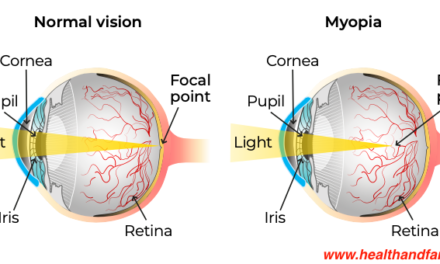
Screening everyone regardless of TB symptoms is game-changing
100 Days focussed campaign is finding more TB in high risk and other vulnerable populations, which includes people living in remote and underserved areas, those who are undernourished, people living with HIV, people with diabetes, and close contacts of people with active TB disease, or those who smoke tobacco or use alcohol.
The 100 days campaign is to find more TB and link them to TB treatment, care and support services, as well as help manage the risk factors (such as, diabetes, undernourishment, etc) and provide TB preventive therapy to those who do not have active TB disease.
Game-changing approach is to screen everyone for TB and not just those with the 4 TB symptoms (cough that lasts more than 3 weeks, loss of appetite and unintentional weight loss, fever, and night sweat). This is based on scientific evidence and India’s National TB Prevalence Survey 2019-2021, and sub-national TB prevalence surveys. India’s survey had found that almost half of the TB patients were asymptomatic and could only be found when screened with X-rays.
Lab On Wheels: Where LOW is the new high
Laboratory on wheels approach has been deployed in finding TB cases in remote settings across the world since many years. For example, World Health Organization (WHO) documented how WHO recommended decentralised, laboratory independent, battery operated and point-of-care Truenat molecular test along with X-rays have been going in a van in Timor-Leste since 2-3 years to reach the unreached people and offer them the best of TB services.
Likewise, in the past 10 years Medanta’s van on wheels initiative has screened over one million people in Delhi and Haryana states with X-rays and linked those with TB disease to public TB services.
India’s Health Minister JP Nadda highlighted government’s new strategies to “make TB services patient-friendly and decentralised. Government has significantly scaled up diagnostic services by increasing the number of laboratories from 120 in 2014 to 8,293 laboratories today.”
Dr Randeep Guleria, former Director of All India Institute of Medical Sciences and a noted respiratory medicine expert and Director of Medanta Medical School wrote a few weeks ago: “From a few hundred molecular test machines in 2014-2015, India now has over 7,700 machines. Truenat, an indigenous molecular diagnostic machine, has drastically reduced the costs of testing, and the time taken to diagnose a patient at district/ block levels.”
As part of India’s 100 days campaign, vans known as “Ni-kshay Vaahan” are taking TB services closer to the people in difficult to reach areas. These vans are fitted with ultraportable handheld X-ray machines that are artificial intelligence enabled and use computer-aided detection for TB. The indigenously built handheld X-ray machine Prorad is among the X-rays which are being deployed in several such settings across the country.
Impacting change
In Barpeta district of western Assam state in India, a photograph shared by government’s National Health Mission (NHM) speaks more than a thousand words: WHO recommended Truenat point-of-care molecular test machine kept on a small wooden bench in an open area is providing state-of-the-art testing for active TB disease and rifampicin drug resistance within an hour to those who would otherwise be left behind. We can also see Ni-Kshay Vahaan in the background.
Uttar Pradesh (UP) Chief Minister told ANI at the start of 2025 that “To make India free from TB, the testing of TB patients in UP has increased 4 times in the last few years. The number of Truenat tests and X-ray machines has also increased.”
In the mountainous state of Himachal Pradesh, vans on wheels are going to far and difficult to reach areas and taking TB diagnostics and services closer to the people. For example, in Deol village near Baijnath (Kangra district), 89 people from key and other vulnerable populations were screened for TB in one day using handheld ultraportable X-ray machines provided by Power Grid Corporation of India (public sector undertaking). Kangra has found 35 more people with active TB disease when it screened thousands with ultraportable handheld X-ray machines and tested over 2000 people from key and other vulnerable populations by 2 January 2025.
Similarly, in Village Hall Keri in Ponda, Goa, 113 people from key and other vulnerable populations were screened with ultraportable X-rays and 37 of those with presumptive TB were referred for molecular testing in one day (on 2nd January 2025). In Bablyakhali and Nagamashid slum area, 89 people were screened with X-rays on the same day. In another camp held in Aam Cottombi, Quepem on 31st December 2024, out of all those screened with X-rays for TB, 40 people were found with presumptive TB and referred for Truenat molecular testing. Goa state is the first state in India which replaced microscopy 100% with upfront molecular testing 3 years back. WHO calls for 100% replacement of microscopy with molecular tests because microscopy underperforms in diagnosing TB.
In 2012, India had made it compulsory for private healthcare facilities to notify TB disease to the government. “This might look like a small step, but it has led to an 8-fold increase in the rate of TB notifications in the private sector,” said JP Nadda, India’s current Health Minister.
Government of India has been providing INR 500 per month to those with TB to support their nutrition for the duration of the treatment (money is directly transferred in the bank account of the patient). Recently this amount has been increased to INR 1000 from 1st November 2024 onwards. Indian Health Minister said that India has transferred over INR 30 billion so far as part of this scheme.
TB rates in India declined by 17.7% and TB death rates came down by 21.4% during the period 2015-2023. As per the latest WHO Global TB Report 2024, India has the highest TB burden in the world (with an estimated 2.8 million people with TB in 2023). India was able to diagnose and offer free treatment to over 2.4 million in 2023. Out of those diagnosed with TB, 32% were diagnosed using upfront molecular testing. It is important to diagnose 100% people with TB with a WHO recommended molecular test, offer latest TB effective TB regimens for treatment, and full cascade of care and support.
Shobha Shukla, Bobby Ramakant – CNS (Citizen News Service)