Situation at a Glance
Description of the Situation
Since the beginning of 2023, and as of 25 February 2024, a total of 13 countries in the WHO African Region have documented probable and confirmed cases of yellow fever (YF), namely Burkina Faso, Cameroon, the Central African Republic, Chad, Republic of the Congo, Côte d’Ivoire, the Democratic Republic of the Congo (DRC), Guinea, Niger, Nigeria, South Sudan, Togo and Uganda.
Preliminary data for 2023 indicate a case fatality rate (CFR) of 11% and a sex ratio of 1.7 (M: F). The median age of cases is 25 years, with two-thirds (69%) of cases aged over 15 years. Suboptimal surveillance capacity exists in many affected countries, with data fragmentation, limited integration with routine surveillance and clinical systems, and a lack of standardized case definitions that contribute to underreporting and increased mortality rates.
During the last quarter of 2023 and as of 25 February 2024, a total of eight countries (Cameroon, Chad, Congo, DRC, Guinea, Niger, Nigeria, and South Sudan), have reported active YF transmission with confirmed YF cases (Table 1). These countries have initiated response planning activities.
Chad, Gabon, Niger, Nigeria, and Togo** are currently awaiting the final classification of the YF laboratory plaque reduction neutralization test (PRNT) positive samples.
Cameroon: Three YF cases were confirmed by polymerase chain reaction (PCR) testing, occurring in the weeks ending on 22 October and 13 November 2023. The country recorded probable and confirmed YF cases consistently throughout 2023, starting from the week ending 29 January 2023.
Chad: A yellow fever PCR-positive case with negative serology was reported on 18 January 2024 from a patient sampled on 10 October 2023, in the Léré district of the Mayo-Kebbi Ouest region.
Republic of the Congo: Cases pending classification with the national health authorities. No further information was available as of February 2024.
Democratic Republic of the Congo: One YF PCR-positive case with unknown vaccination status was reported on 18 December 2023. Additionally, nine PRNT positive cases were recorded, eight of which have unknown vaccination status and one lacks information in the medical charts.
Guinea: Three YF PCR-positive cases were confirmed at the Institute Pasteur Dakar (IPD). These cases were reported on 17 October and 23 December 2023 in a 6-year-old female from Faranah region, a 7-year-old male from the Koundara health district (sample collected on 6 December), and a 60-year-old female from the Guiéckédou district (sample collected on 15 December), representing three out of the seven country’s regions. Notably, this occurrence is less than three years since cases were confirmed in the Koundara health district in 2020 and 2021.
Niger: Case reported in the Tahoua city, Department of Tahoua during the first week of January 2024. No further information was available as of February 2024. Investigations are ongoing.
Nigeria: One YF PRNT-positive case was reported in January 2024 in Lagos state in a 49-year-old male residing in a rural area. Investigations are ongoing.
South Sudan: A confirmed YF case was reported on 24 December 2023, following the investigation of suspected cases and deaths of viral hemorrhagic fever. The case, a 24-year-old male, presented with fever, vomiting blood, and jaundice. Two additional cases were confirmed on 2 February 2024. As of 12 February 2024, South Sudan reported a total of 64 cases that fulfil the current outbreak case definition of YF, including 61 suspected cases and three confirmed cases from six out of 10 counties in Western Equatoria state: Yambio (33), Nzara (09), Tambura (12), Ibba (4), Ezo (5) and Maridi Counties (1). Among 61 suspected cases, there were six suspected deaths currently under investigation.
Figure 1. Distribution of reported confirmed yellow fever cases in eight countries in the WHO African Region between 1 October 2023 (EW40/2023) and 21 February 2024 (EW8/2024)

Table 1. Classification of reported confirmed yellow fever cases by country in the WHO African Region based on regional reference laboratory results and outputs of classification sessions, from 1 October 2023 (EW40/2023) to 21 February 2024 (EW8/2024).
Footnotes:
PRNT: Plaque reduction neutralization test
RT-qPCR: quantitative reverse transcriptase-polymerase chain reaction
Confirmed case: a confirmed case of yellow fever virus infection by a positive RT-qPCR result
* Of note, during 2023, Cameroon reported 32 confirmed cases from all 10 country regions, including 23 PRNT-positive and nine RT-PCR-positive cases. Among the six PRNT positive samples, four were rejected. Notably, six cases were classified as confirmed within Douala’s densely populated urban area during Epi Weeks 8 – 38 of 2023.
¥ Not available
** Kindly note that one case in Togo is pending classification
Togo – EW 5 (29 Jan 2024) – During EW5, a 7-year-old female presented to the health care facility with fever and jaundice with no other symptoms. The child was vaccinated against YF , fife years before and had no history of travel. Laboratory results showed a positive rapid diagnostic test for malaria, and she was treated accordingly. In addition, she presented a YF-PRNT result of 1/60. The child fully recovered from symptoms. This case is pending case classification with the Ministry of Health.
Epidemiology
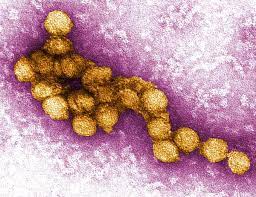
Yellow fever is an epidemic-prone, vaccine-preventable disease caused by an arbovirus transmitted to humans primarily through the bites of an infected Aedes spp. and Haemagogus spp. mosquitoes. The incubation period ranges from 3 to 6 days. Many people do not experience symptoms, but when they occur, the most common are fever, muscle pain with prominent back pain, headache, loss of appetite, and nausea or vomiting. In most cases, symptoms disappear after 3 to 4 days. A small percentage of cases progress to a toxic phase with systemic infection affecting the liver and kidneys. These individuals can have more severe symptoms of high-grade fever, abdominal pain with vomiting, jaundice and dark urine caused by acute liver and kidney failure. Bleeding can occur from the mouth, nose, eyes, or stomach. Death can occur within 7 to 10 days in about half of cases with severe symptoms.
Yellow fever is prevented by an effective vaccine, which is safe and affordable. A single dose of yellow fever vaccine is sufficient to grant sustained immunity and life-long protection against yellow fever disease. A booster dose of the vaccine is not needed. The vaccine provides effective immunity within 10 days for 80-100% of people vaccinated, and within 30 days for more than 99% of people vaccinated.
Public Health Response
To respond to yellow fever outbreaks, regional and national public health measures have been organized across several domains.
Coordination – Countries have developed and rolled out national response plans aimed at tackling YF outbreaks with a focus on preventive measures, improved surveillance, and reactive vaccination campaigns. As per its strategy, the global Eliminate Yellow Fever Epidemics (EYE) secretariat led the coordination of significant preventive and reactive efforts and, notably, during 2023, substantially enhanced vaccination coverage. Approximately 62 million people have been protected in Africa through PMVC and reactive mass vaccination campaigns (RMVC). Also, approximately 17.4 million children are protected through Routine Immunization in Africa. The WHO Regional Office for Africa, in conjunction with the EYE Strategy Secretariat, is supporting countries in their efforts to prevent and respond to YF outbreaks.
Surveillance – Efforts have been bolstered in some countries including Cameroon, the Central African Republic and Guinea, to enhance their systems for the early detection and monitoring of cases. This includes conducting root cause analyses to understand the factors driving outbreaks and performing immunity gap analyses to pinpoint vulnerable population groups for targeted vaccination efforts.
Case Management and Vector control – Improvements have been made in capacity building for the clinical case management and measures for prevention and control have been enhanced nationally in the most affected countries. Vector control activities have also been planned in urban areas with confirmed YF cases to curb further spread.
Laboratory testing – There has been a significant strengthening of capabilities. National reference laboratories have enhanced YF IgM testing and PCR diagnosis capacities in some countries, complemented by regional reference laboratories for confirmatory testing. This strengthening extends to national and regional levels, facilitated by EYE strategy operations.
Vaccination – Vaccination campaigns form a crucial pillar in the YF outbreak response.
In 2023, nearly 62 million individuals received vaccinations under the EYE strategy. This comprised 57.2 million reached through Preventive Mass Vaccination Campaigns (PMVCs) in the Democratic Republic of the Congo, Nigeria, and Uganda, along with 686 405 individuals vaccinated through reactive campaigns in areas including the Central African Republic (Mbaiki), Guinea (Dabola district and Dinguiraye), and Niger (Gazaoua). Additionally, approximately 4 million individuals received vaccination against YF under catch-up campaigns in Sudan. All International Coordination Group (ICG) requests for vaccination have been met with funding and technical support, ensuring a timely vaccine supply to affected countries.
Risk Communication and Community Engagement – These involve targeted communication strategies to enhance awareness about YF risks, preventive measures, and the importance of vaccination, especially targeting hard to reach populations such as nomads, refugees, forest workers, and internally displaced persons. Engagement with these communities is being prioritized to ensure a comprehensive understanding of YF risks and the benefits of vaccination.
This multi-faceted approach, which covers coordination, surveillance, case management, laboratory enhancement, vaccination, vector control and community engagement, underscores the essential components of the public health response to Yellow Fever outbreaks.
Despite these robust measures, certain vulnerabilities remain. These include the challenge of competing outbreaks which may divert resources and delay response efforts, surveillance and laboratory challenges characterized by inadequate logistics, poor sample collection, and lengthy diagnostics turnaround times, and observed delays in reactive vaccination following yellow fever cases and submissions of ICG requests.
As of 4 March 2024, WHO is providing technical support to the national health authorities of Burkina Faso, Cameroon, Congo, DRC, South Sudan and Togo to assess the final classification of cases.
WHO Risk Assessment
As part of the ongoing efforts to monitor and respond to infectious disease outbreaks, on 12 February 2024, the World Health Organization conducted a Rapid Risk Assessment for yellow fever. It aimed to reassess the current regional risk of multiple ongoing YF outbreaks, in the context of a resurgence of YF outbreaks in countries with a history of preventive vaccination campaigns and persisting immunity gaps, including capacities to support the response (e.g., technical capacities, vaccine supply and vaccination campaigns, laboratory and operations, support and logistics (OSL)) and to provide recommendations for a more effective and coordinated response.
The overall risk at the regional level was re-assessed as moderate based on several contributing factors observed in the region despite the efforts to control the spread of YF:
- Stable number of ongoing outbreaks across the region.
- Persistence of pockets of unimmunized populations although considerable efforts have been made in recent years to protect the population through PMVC and reactive mass vaccination campaigns (RMVC).
- Detection of YF confirmed cases in urban areas, such as Douala city in Cameroon, which pose significant risks due to high population density and international travel connections, noting nevertheless the risk mitigation provided by a relatively high average vaccination coverage
- Risk of cross-border spread, particularly from the outbreak in South Sudan, which shares borders with neighbouring countries.
- Limited surveillance and laboratory capacity in certain regions may result in delayed detection, underestimation of the extent of the disease and delayed response.
- Persisting response challenges with the case classification, investigation, and response operations, exacerbated by competing health emergencies.
- Competing outbreaks strainthe capacity to respond effectively, with various simultaneous health crises, including measles, poliomyelitis, mpox, cholera, diphtheria, hepatitis E, Lassa fever, and dengue. These challenges are compounded by factors such as food insecurity, security constraints, and complex humanitarian contexts. Furthermore, public health and medical personnel are overburdened, managing multiple parallel outbreaks alongside other health emergencies.
- Socio-economic factors, high levels of poverty and limited resource allocation contribute to the challenge of controlling outbreaks effectively.
While the global risk remains low, active surveillance is required due to the potential for onward transmission through viremic travellers and the presence of the competent vector in neighbouring regions.
While progress has been made in controlling outbreaks, ongoing challenges and vulnerabilities underscore the need for sustained and coordinated efforts to protect public health. The impact on public health will persist until the ongoing outbreaks are controlled, vaccination coverage is high and immunity gaps in the population closed. The importation of cases to countries with suboptimal coverage and persisting population immunity gaps poses a high risk and may jeopardize the tremendous efforts invested to achieve elimination.
WHO Advice
Yellow Fever is an epidemic-prone mosquito-borne vaccine- preventable disease transmitted to humans by infected mosquitoes, notably Aedes sp. and Haemagogus species. The urban proliferation of Aedes spp. mosquitoes (day feeders)) can significantly amplify transmission risks, particularly in densely populated areas, leading to swift outbreaks.
Surveillance and Coordination: WHO emphasizes the importance of active surveillance, cross-border coordination, and information sharing. Investigating and testing suspected cases is crucial for outbreak control and prevention. Enhanced surveillance with investigation and laboratory testing of suspect cases is recommended.
Vaccination as a Primary Prevention Tool: Vaccination is the primary means for prevention and control of YF. The WHO’s EYE strategy prioritizes vaccination in countries reporting YF, integrating it into routine immunization schedules for individuals aged 9 months and above. Proof of vaccination is required for travellers to and from countries with YF risk, with specific exemptions. The WHO supports the expansion of vaccination coverage through routine programs and mass vaccination campaigns to enhance communal immunity.
Guidance for International Travelers: All international travellers aged 9 months and above heading to areas at risk of YF transmission, as determined by WHO, are advised to get vaccinated. The vaccine is deemed safe and effective, offering life-long protection. However, vaccination recommendations for infants under 9 months, and pregnant or breastfeeding women are nuanced, advocating for vaccination in high-risk scenarios after weighing the benefits against potential risks.
Regulatory Aspects and Vaccine Validity: Under the International Health Regulations (IHR 2005), countries have the autonomy to require proof of YF vaccination from incoming travellers. The International Certificate of Vaccination or Prophylaxis (ICVP) must document this vaccination, with validity extending throughout the vaccinated individual’s lifetime. WHO-approved YF vaccines guarantee lifelong immunity, negating the need for booster doses for international travel.
Vector Control and Risk Communication: Effective vector control in urban settings and general mosquito bite avoidance strategies are recommended to prevent disease transmission. WHO urges Member States to inform travellers about YF risks, preventive measures, and to seek immediate medical attention if symptoms arise. This approach helps prevent the establishment of local transmission cycles through infected travellers.
International Travel and Trade: WHO advises against imposing travel or trade restrictions related to YF. Continuous efforts to educate travellers on preventive measures, including vaccination, are encouraged.
Additional Recommendations: Given the evolving nature of YF transmission, WHO advises Member States to remain updated with the latest information and guidelines available on the WHO International Travel and Health website. Local health authorities are encouraged to collaborate closely with WHO and other relevant stakeholders to implement effective YF prevention and control measures, ensuring the safety and well-being of populations at risk.
Further Information
- World Health Organization (3 January 2023). Disease Outbreak News; Yellow fever in East, West, and Central Africa. Available at: https://www.who.int/emergencies/disease-outbreak-news/item/2022-DON431
- WHO YF fact sheet: http://www.who.int/news-room/fact-sheets/detail/yellow-fever
- WHO strategy for YF epidemic preparedness and response: https://www.who.int/initiatives/eye-strategy
- Laboratory Manual for Yellow Fever (https://www.who.int/publications/i/item/9789240084476)
- Countries with risk of yellow fever transmission and countries requiring yellow fever vaccination (November 2022): https://www.who.int/publications/m/item/countries-with-risk-of-yellow-fever-transmission-and-countries-requiring-yellow-fever-vaccination-(november-2022)
- Vaccination requirements and recommendations for international travellers; and malaria situation per country – 2022 edition: https://www.who.int/publications/m/item/vaccination-requirements-and-recommendations-for-international-travellers-and-malaria-situation-per-country-2022-edition
- A Global Strategy to Eliminate YF Epidemics (EYE), document for SAGE –October 2016 https://www.who.int/news-room/events/detail/2016/10/18/default-calendar/strategic-advisory-group-of-experts-on-immunization-(sage)—october-2016
- SAGE: https://www.who.int/groups/strategic-advisory-group-of-experts-on-immunization/
- Meeting of the Strategic Advisory Group of Experts on Immunization, October 2016: conclusions and recommendations. Weekly Epidemiological Record, 91 (48), 561 – 582. https://www.who.int/publications/i/item/WER9148
- A Global strategy to Eliminate YF Epidemics (EYE) 2017-2026, WHO 2018, http://apps.who.int/iris/bitstream/handle/10665/272408/9789241513661-eng.pdf?ua=1
- WHO – International Travel and Health website: https://www.who.int/health-topics/travel-and-health#tab=tab_1
- WHO – YF – West and Central Africa https://www.who.int/emergencies/disease-outbreak-news/item/yellow-fever—west-and-central-africa
Citable reference: World Health Organization (20 March 2024). Disease Outbreak News; Yellow fever in African Region (AFRO). Available at: https://www.who.int/emergencies/disease-outbreak-news/item/2022-DON510