Ahead of World Malaria Day, the WHO Global Malaria Programme published a new operational strategy outlining its priorities and key activities up to 2030 to help change the trajectory of malaria trends, with a view to achieving the global malaria targets. The strategy outlines 4 strategic objectives where WHO will focus its efforts, including developing norms and standards, introducing new tools and innovation, promoting strategic information for impact, and providing technical leadership of the global malaria response.
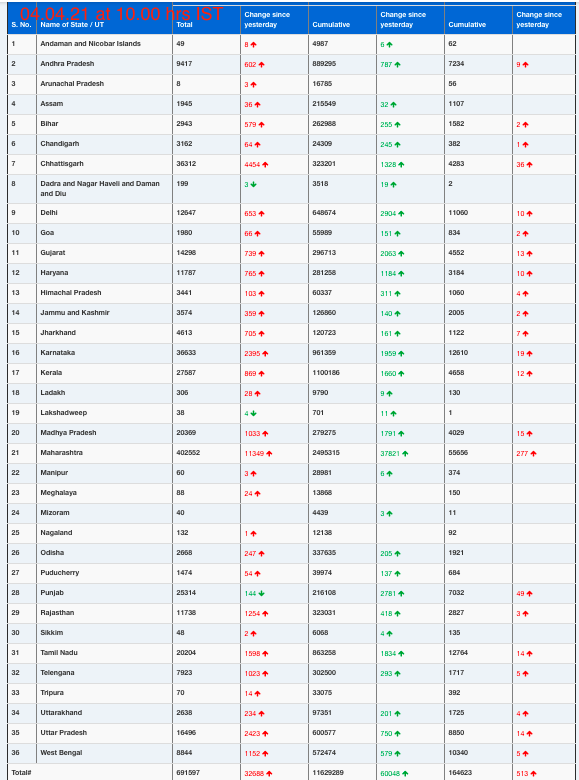
In recent years, progress towards critical targets of the WHO Global technical strategy for malaria 2016-2030 has stalled, particularly in countries that carry a high burden of the disease. In 2022 there were an estimated 608 000 malaria-related deaths and 249 million new malaria cases globally, with young children in Africa bearing the brunt of the disease.
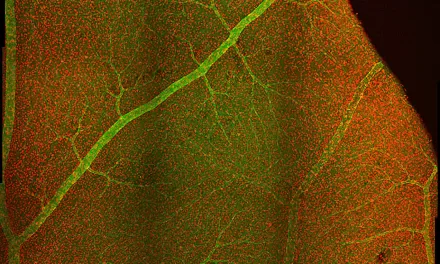
Millions of people continue to miss out on the services they need to prevent, detect, and treat malaria. Additionally, progress in global malaria control has been hampered by resource constraints, humanitarian crises, climate change and biological threats such as drug and insecticide resistance.
“A shift in the global malaria response is urgently needed across the entire malaria ecosystem to prevent avoidable deaths and achieve the targets of the WHO global malaria strategy,” notes Dr Daniel Ngamije, Director of the Global Malaria Programme. “This shift should seek to address the root causes of the disease and be centred around accessibility, efficiency, sustainability, equity and integration.”
Strategic objectives
The WHO Global Malaria Programme has an important role to play in leading the response to control and eliminate the disease worldwide. Through its direct actions and networks, including a presence in 150 countries, the Programme is well placed to shape the malaria ecosystem and achieve impact at country level.
The new operational strategy includes 4 strategic objectives.
- Develop and disseminate norms and standards. Evidence-based technical recommendations are a cornerstone of the fight against malaria. Normative guidance supports the translation of evidence into action by aligning countries and partners under one common technical vision and strategic direction. The Global Malaria Programme has a core responsibility to guide the research agenda and analyse evidence that can inform global policy.
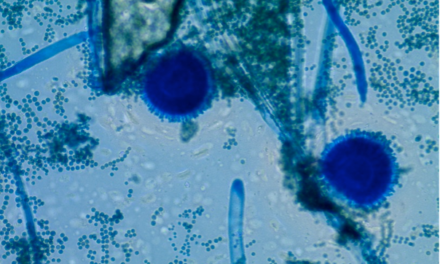
- Stimulate the development and timely introduction of new tools and innovation. While more progress can be achieved with currently available tools, new interventions are needed to accelerate the gains and counter emerging threats. The Global Malaria Programme plays a critical key role in facilitating the evaluation and introduction of new malaria control tools and works closely with multiple partners to provide an evidence base to inform their effective scale-up.
- Promote the use of strategic information for impact. The Global Malaria Programme’s work in monitoring, evaluating and reporting on trends in malaria burden, control and elimination drives priorities and decision-making at all levels – from in-country actors to international donors and other partners. WHO’s work also includes global and national equity monitoring as well as support for local barrier assessments to better understand who is missing out on malaria interventions.
- Provide technical leadership of the global malaria response. WHO leads and coordinates the United Nations’ health agenda at both the country and global levels. The Organization has a core responsibility to convene key stakeholders, define and advocate for priority activities, and empower communities and individuals to access quality health services. The Global Malaria Programme embodies this core WHO function in the malaria ecosystem.
Guiding principles
The new operational strategy is guided by 3 equity-oriented principles:
- Country ownership and leadership, with a whole-of-government and whole-of-society approach. Efforts to fight malaria must be fully owned and led by countries with adequate investment of domestic resources and a multisectoral response. A country-led response further promotes inclusive governance, accountability and specific interventions that are tailored to local contexts.
- Resilient health systems to enable the success of national malaria responses. Ensuring the provision of malaria services relies on a strong primary health care system that can respond to emerging needs and provide quality care for all people, including those infected with malaria.
- Equity in access to quality health services. All efforts to fight malaria should be rooted in the principles of equity, gender equity and human rights to ensure that the most vulnerable are protected and have access to quality health services, including malaria interventions and information.
Equity in access to malaria services is the focus of the year’s World Malaria Day under the theme: “Accelerating the fight against malaria for a more equitable world.” It is also a central tenet of the Yaoundé Declaration, signed in March 2024 by African Ministers of Health from some of the countries hardest hit by malaria.
In signing the declaration, Ministers committed, among other measures, to the aim of ensuring that all populations at risk of malaria consistently receive the appropriate tools – including those living in hard-to-reach areas and conflict humanitarian settings.