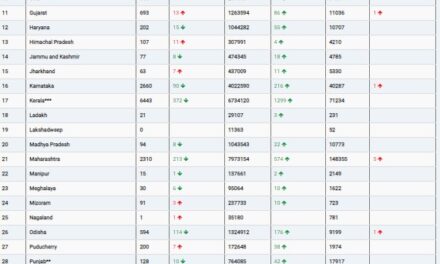
The data suggests that there is variability in antimicrobial prescribing among hospital-based physicians, but this variation is not associated with patient characteristics or clinical outcomes. In a multicenter study involving 124 physicians responsible for over 124,000 hospitalized patients, the difference in mean prescribing between the highest and lowest quartiles of prescription volume was 15.8 days of treatment per 100 patient-days.
Patient characteristics were similar across the quartiles, and there were no significant differences in patient outcomes, including in-hospital deaths, hospital length of stay, intensive care unit transfer, and hospital readmission. This lack of association between prescribing levels and outcomes surprised the researchers.
The study’s lead author, Mark T. McIntyre, emphasized that this research does not define the quality of care provided by physicians. Instead, it highlights the natural variation in prescribing practices and their limited association with patient outcomes. McIntyre suggests that factors such as comfort level, risk tolerance, and social, cultural, and contextual factors likely influence prescribing practices.
The study, published in the Canadian Medical Association Journal, suggests that there may be opportunities to optimize antimicrobial prescribing in ways not previously considered. It raises questions about what drives prescribing practices and how they can be improved.
The study used a retrospective cohort design and evaluated physician-level volume and spectrum of antimicrobial prescribing in adult general medical wards across four academic hospitals in Toronto, Canada, from 2010 to 2019. Physicians were stratified into quartiles based on the volume and spectrum of their antimicrobial prescribing. Patient characteristics were balanced across the quartiles.
The study found no significant differences in clinical outcomes based on quartiles of prescribing volume or spectrum after adjusting for patient-level characteristics. In-hospital mortality was slightly higher among patients cared for by prescribers with higher modified spectrum scores, but this finding was not consistent across all analyses.
The authors concluded that reducing antimicrobial exposure, without a discernible benefit in patient outcomes, may be possible and could contribute to lower antimicrobial resistance.
Commenting on the study, Dr. Lawrence I. Kaplan, an expert in general internal medicine, suggested that achieving the lowest quartile of prescribing could be a goal, and there’s a need for better training in clinical management decision-making. He proposed the use of clinical decision-making tools integrated into electronic health records to guide appropriate antibiotic use based on evidence.
Kaplan emphasized the importance of interdisciplinary collaboration and the role of pharmacists in assisting with treatment decision-making and identifying potential drug interactions.
In summary, the study highlights the variability in antimicrobial prescribing among hospital physicians and the need to explore ways to optimize prescribing practices, with a focus on evidence-based decision-making and interdisciplinary collaboration.