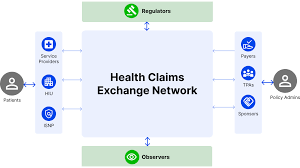
The Government of India has announced a significant milestone in the health insurance sector with the ongoing implementation of the National Health Claims Exchange (NHCX). This innovative gateway, developed under the Ayushman Bharat Digital Mission (ABDM), aims to revolutionize health insurance claim processing by standardizing and accelerating the procedure, thereby enhancing efficiency within the insurance industry and improving the patient experience.
As of today, 34 insurers and Third-Party Administrators (TPAs) have successfully integrated with NHCX. Additionally, around 300 hospitals are gearing up to commence sending their claims through this new system. This integration is set to streamline the exchange of health claim information among insurers, TPAs, healthcare providers, beneficiaries, and other relevant entities, ensuring interoperability, machine-readability, auditability, and verifiability.
Key Benefits of NHCX:
- Standardized Processing: By providing a standardized framework, NHCX will enable faster and more consistent processing of health insurance claims. This reduces administrative burdens and the potential for errors, leading to quicker settlements.
- Enhanced Efficiency: The system’s design ensures efficient handling of claims, from submission to settlement. This efficiency translates into cost savings for insurers and improved service for policyholders.
- Improved Transparency: NHCX enhances transparency within the insurance ecosystem. Policyholders will benefit from clear and traceable claim processing, fostering greater trust in the system.
- Interoperability: The platform ensures seamless data exchange across various entities involved in health insurance, facilitating smoother operations and reducing information silos.
Supported by the Insurance Regulatory and Development Authority of India (IRDAI) and the General Insurance Council (GIC), NHCX represents a significant step forward in India’s digital health journey. The exchange is part of the broader Ayushman Bharat – Pradhan Mantri Jan Arogya Yojana (AB-PMJAY), which provides health coverage of Rs. 5 lakh per family per year for secondary and tertiary care hospitalization. This scheme covers 55 crore individuals, corresponding to 12.34 crore families, offering comprehensive health protection to eligible families, regardless of age.
In a written reply to the Lok Sabha, the Union Minister of State for Health and Family Welfare, Shri Prataprao Ganpatrao Jadhav, emphasized the transformative impact of NHCX on the healthcare and insurance sectors. “This initiative marks a significant leap towards ensuring efficient and transparent health insurance processes, ultimately benefiting policyholders and healthcare providers,” he stated.
The rollout of NHCX is a testament to the government’s commitment to leveraging digital technology to enhance public welfare. As more hospitals join the platform and insurers adapt to the new system, the anticipated improvements in claim processing times and accuracy will become increasingly evident, marking a new era in India’s health insurance landscape.