In a groundbreaking exploration shedding light on postpartum maternal health, researchers at UC Santa Barbara have uncovered a correlation between the immune status of postpartum mothers and how they feed their infants. The study, published in Scientific Reports, delves into the fluctuations of inflammatory proteins in relation to breastfeeding, pumping, or formula-feeding practices.
Led by Amy Boddy, a human biologist and evolutionary theorist at UCSB’s Department of Anthropology, the study marks a significant departure from the conventional focus on infant health outcomes associated with breastfeeding. “It’s a great study; there are so many unanswered questions about maternal health in the postpartum period,” expressed Boddy, highlighting the critical need for research from the perspective of mothers.
The research, conducted in collaboration with co-Principal Investigator Carmen Hové and their team, monitored 96 postpartum women in the Seattle area, gathering saliva samples over a 24-hour period. This period encompassed pre-sleep and post-wake cycles, offering insights into the diurnal patterns of five inflammatory proteins (CRP, IL-1β, IL-6, IL-8, and TNF-α) associated with immune response.
The unexpected advantage of the COVID-19 lockdown provided an ideal experimental setting, minimizing environmental factors that could confound immune readings. “It was kind of a perfect natural experiment because we’re looking at immune function, and none of the participants were sick,” Boddy remarked, underscoring the controlled environment.
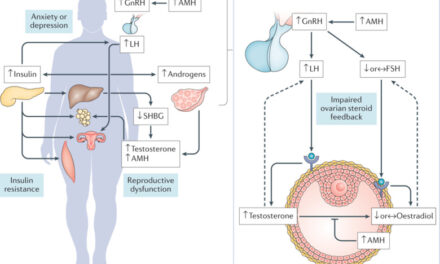
The study’s findings revealed intriguing shifts in inflammatory protein levels, particularly in the case of C-reactive protein (CRP), which peaked in the evenings for mothers heavily reliant on breastfeeding, contrary to the typical diurnal trend. Hové noted, “Among mothers who reported intensive lactation, via either breastfeeding or pumping, CRP was higher at nighttime,” emphasizing the need for further research to decipher the implications of this unique pattern.
Boddy postulated several potential explanations for the observed phenomena, ranging from incomplete breast emptying leading to inflammation to stress-induced behavioral changes affecting breastfeeding patterns. However, she cautioned against drawing definitive conclusions without further investigation.
The study’s significance lies in its illumination of the intricate dynamics of postpartum breastfeeding, underscoring the evolutionary tug-of-war between maternal and infant needs. Boddy explained, “There’s something in evolutionary biology called maternal-fetal conflict… the baby always wants a little more than the mother has to give,” highlighting the nuanced interplay between maternal health and breastfeeding practices.
Despite societal endorsements of breastfeeding, the study uncovered a diversity of lactation feeding strategies among participants, reflecting the challenges faced by mothers, even within educated and affluent demographics. Boddy herself, reflecting on her own breastfeeding journey, acknowledged the demanding nature of breastfeeding and the societal constraints hindering lactational support.
Moving forward, the researchers aim to delve deeper into individualized postpartum health and breastfeeding patterns, particularly focusing on hormonal dynamics. “This study has opened up more questions than what we’ve answered… It’s always been challenging to find the best way of feeding our babies,” Boddy concluded, underscoring the ongoing quest for a comprehensive understanding of postpartum maternal health.