Situation at a glance
The Ministry of Health and Population (Ministère de la Santé et de la Population – MSP) of the Republic of the Congo, declared on 17 July 2023 a suspected triple outbreak of gastroenteritis, with typhoid fever, shigellosis, and cholera as probable causes.
Since the first case was reported on 28 June 2023, and as of 29 August 2023, a total of 2389 suspected cases have been reported, including 52 deaths (overall Case Fatality Rate (CFR) 2.2%).
Laboratory analyses performed by the National Public Health Laboratory, identified 83 cases of Shigella, 22 of Salmonella Typhi (S. Typhi) and 21 cases of Vibrio cholerae with toxigenicity testing of the strain not performed.
The city of Dolisie, the capital of Niari Department in the western part of the country is the epicentre of this outbreak.
With WHO support, the MSP has activated a multisectoral coordination mechanism, strengthening surveillance, laboratory and clinical care capacities, and implementing decontamination and risk communication activities. An in-depth epidemiological investigation is also being led by the MSP.
WHO assesses the risk posed by this triple outbreak as high at the national level, moderate at the regional level and low at the global level.
Description of the situation
On 14 July 2023, the Ministry of Health and Population of the Republic of the Congo reported 1384 cases whose dominant symptomatology was fever (39°C and 40°C), headaches, abdominal pain, diarrhoea, vomiting, and fatigue.
On 17 July 2023, the MSP officially declared a suspected triple outbreak of gastroenteritis, with typhoid fever, shigellosis, and cholera as probable causes.
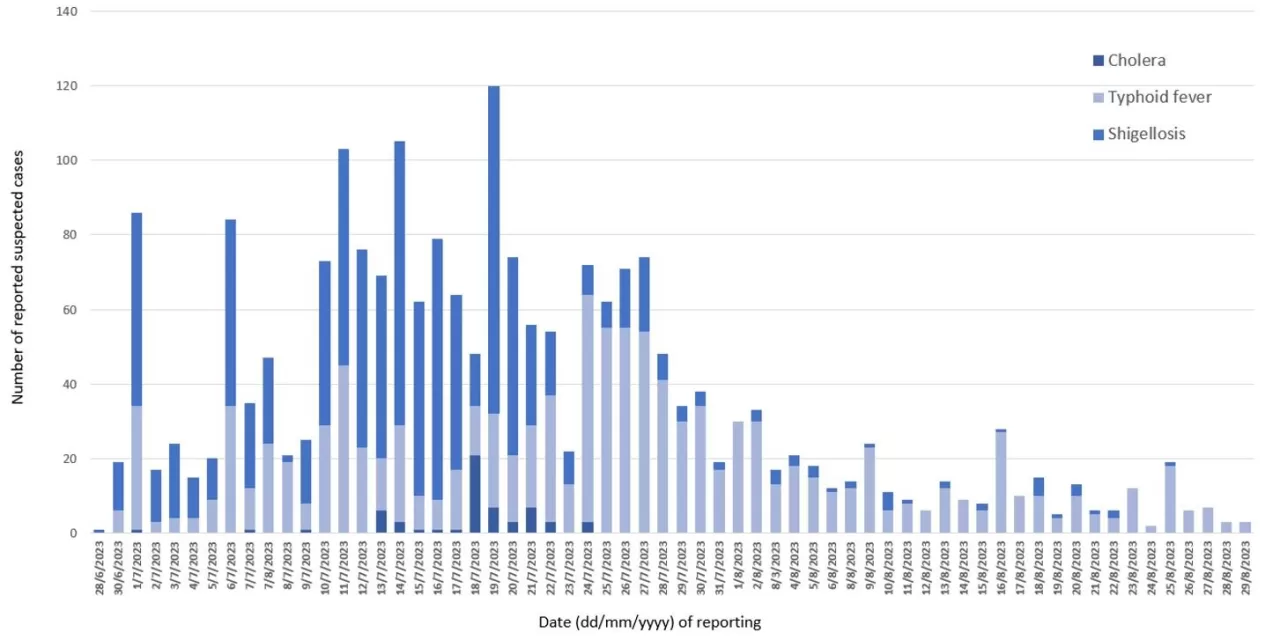
The first case of the outbreak was reported on 28 June 2023. Since then, and as of 29 August 2023, a total of 2389 suspected cases have been reported, including 52 deaths (overall CFR 2.2%). Suspected typhoid fever cases accounted for 50.2% (n=1200) of all cases, followed by shigellosis (46.9%; n=1120) and cholera (2.9%; n=69).
Eighty-eight (3.7%) of the suspected cases have undergone emergency surgery due to an intestinal perforation, a complication known to occur in untreated typhoid fever.
The city of Dolisie – the capital of Niari Department with a population of more than 110 000 inhabitants – is the current epicentre of this outbreak, with 2178 suspected cases (91.2% of all cases) and 33 deaths (CFR 1.5%) reported for all three infectious diseases combined.
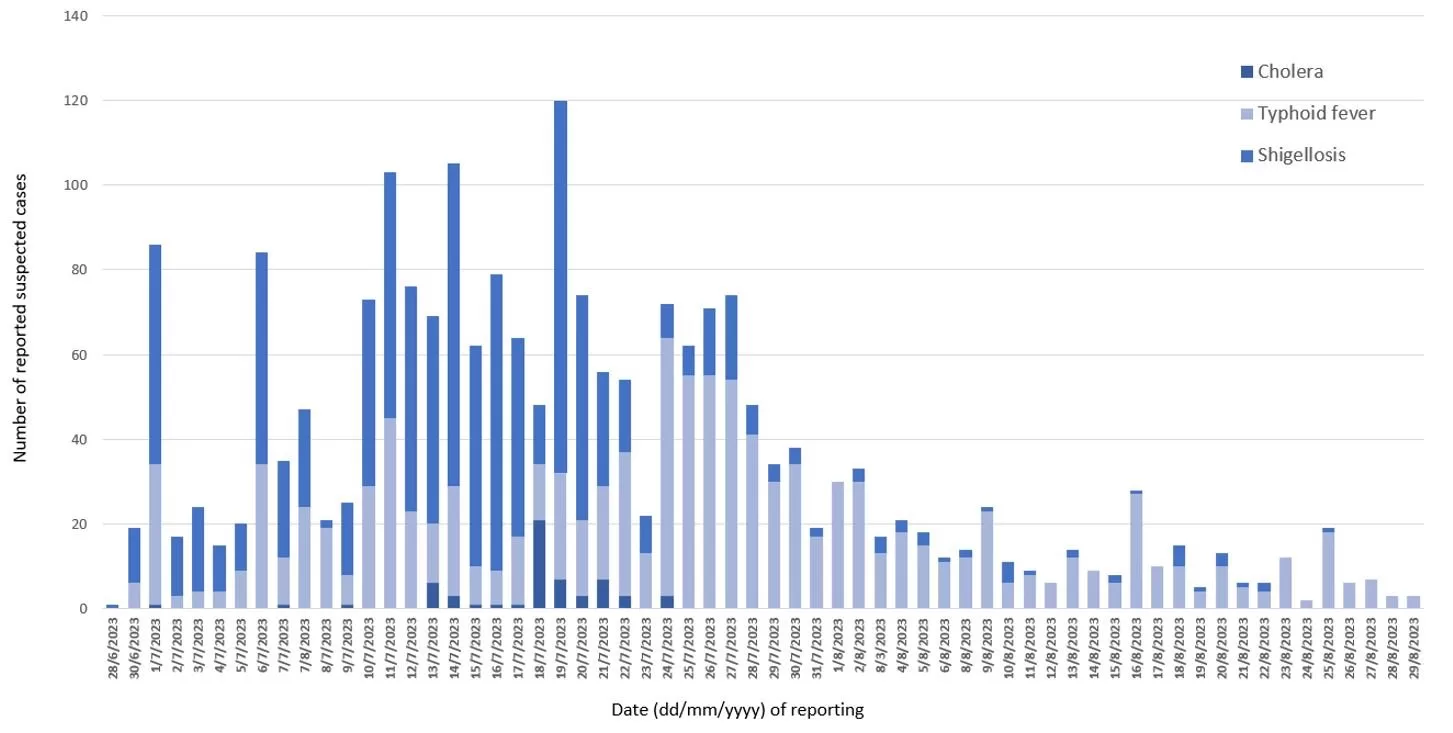
Figure 1. Distribution of suspected cases of typhoid fever, shigellosis, and cholera by date of reporting, Dolise, Niari Department, 28 June – 29 August 2023 (n=2178).
Since the beginning of this outbreak, Dolisie has registered an overflow of health facilities with more than 600 suspected cases admitted during July-August. A reduction in the number of admitted patients has been observed since September.
Five other departments in the Republic of Congo (Bouenza, Brazzaville, Kouilou, Pointe-Noire and Pool) have also reported suspected cases.
Of the 2071 cases (86.7%) with information on age and sex, 51.6% (n=1068) were females, and the most affected age group was 11-20 years (n=674; 32.5%), followed by the 0-10 age group (n=506; 24.4%) and the 21-30 age group (n=403; 19.4%).
Figure 2. Age and sex distribution among suspected cases (n=2071).
The available isolation results from the National Public Health Laboratory (LNSP) are distributed as follows (the number of samples tested is not known):
- Eighty-three confirmed cases of Shigella (flexneri & dysenteriae). The most affected age group is patients between 5 and 30 years old, representing 64% (53/83) of laboratory-confirmed cases of Shigella.
- Twenty-two confirmed cases of Salmonella Typhi. The most affected age group is patients between 5 and 30 years old, representing 59% (13/22) of laboratory-confirmed cases of typhoid fever.
- Twenty-one confirmed cases of Vibrio cholerae, including 11 co-infections with Shigella, and one co-infection with S. typhi. The serogroup typing showed serogroup O1 serotype Inaba for eight out of nine samples for which serotyping was conducted. However, given the prolonged absence of reported cholera in the country (the last documented outbreak was in 2016) and the absence of epidemiological links to other ongoing cholera outbreaks (i.e. in the neighbouring countries of the Democratic Republic of the Congo and Cameroon), toxigenicity testing of the strain is still required to ascertain confirmation of cholera aetiology in accordance with WHO and The Global Task Force on Cholera Control (GTFCC) standards. The most affected age group for confirmed cholera cases is between 5 and 30 years old, representing 76% (16/21) of laboratory-confirmed cases.
The results of the antibiogram conducted on 78 samples of stool analysed, indicated a resistance and/or reduced susceptibility to carbapenems, third generation cephalosporins, and quinolones in several of the reported isolates of Shigella and Salmonella, while most of S. Typhi isolates are reported to be susceptible to ciprofloxacin (the number of the antibiogram results by pathogen and drug is unknown).
Epidemiology of the diseases
Cholera is an acute enteric infection caused by ingesting the bacteria Vibrio cholerae present in contaminated water or food. It is mainly linked to insufficient access to safe drinking water and inadequate sanitation. It is an extremely virulent disease that can cause severe acute watery diarrhoea resulting in high morbidity and mortality, and can spread rapidly, depending on the frequency of exposure, the exposed population and the setting. Cholera affects both children and adults and can be fatal if untreated. The incubation period is between 12 hours and five days after ingestion of contaminated food or water. Most people infected with V. cholerae do not develop any symptoms, although the bacteria are present in their faeces for 1-10 days after infection and are shed back into the environment, potentially infecting other people. The majority of people who develop symptoms have mild or moderate symptoms, while a minority develop acute watery diarrhoea and vomiting with severe dehydration. Cholera is an easily treatable disease. Most people can be treated successfully through prompt administration of Oral Rehydration Solution (ORS).
After decades of progress against cholera, an upsurge has been recorded in several countries since 2021. From 1 January 2023 to 15 August 2023, at least 28 countries have reported cholera cases, compared with 16 countries in the same period of 2022. The WHO African Region is the most affected region with 16 countries reporting cholera cases since the beginning of 2023. In Congo, from 1997 to 2016, a total of six cholera outbreaks have been reported, with the last occurred in Mpouya (Plateaux Department), with 18 cases including three deaths (CFR 16.7%).
Shigellosis is a gastrointestinal infection caused by one of four species of Shigella bacteria (Shigella sonnei, S. flexneri, S. boydii and S. dysenteriae). It is found in the intestinal tract of infected people and can be transmitted through the faecal-oral route by direct or indirect contact (e.g., through flies) with faeces from an infected person, fomites, consumption of contaminated food or water and person-to-person contact. Sustained sexual transmission has become an important component of Shigella species epidemiology. Humans are the only reservoir and can excrete bacteria in their stools for weeks after a dysenteric episode. Adequate antibiotic treatment can reduce the carriage status. Asymptomatic carriers can also contribute to the spread of the disease. Fluoroquinolones, cephalosporins, and azithromycin are recommended to treat more severe cases with underlying conditions or to limit transmission.
Typhoid fever is a life-threatening infection caused by the bacterium Salmonella Typhi. It is usually spread through contaminated food or water. Once Salmonella Typhi bacteria are ingested, they multiply and spread into the bloodstream. Symptoms include prolonged fever, fatigue, headache, nausea, abdominal pain, and constipation or diarrhoea. Some patients may have a rash. Severe cases may lead to serious complications, such as intestinal perforation, or even death. Patients can be treated with antibiotics although increasing resistance to different types of antibiotics is making treatment more complicated. WHO has prequalified two typhoid conjugate vaccines since December 2017 and are being introduced into childhood immunization programs in typhoid-endemic countries.
Public health response
- WHO is supporting the MSP in conducting an in-depth epidemiological investigation of this triple outbreak to better characterize it, particularly the epidemiological profiles of cases of intestinal perforation and deaths.
- A national integrated response plan to shigellosis outbreaks, typhoid fever, and cholera has been developed.
- The MSP activated multisectoral coordination mechanisms at the national level and in the departments of Niari, Kouilou and Bouenza.
- WHO is supporting the MSP in strengthening surveillance in healthcare facilities and communities where the active search for suspected cases is underway. A mobile laboratory was also deployed in Dolisie.
- Environmental monitoring with water quality testing and decontamination of affected water sources is ongoing.
- Risk communication and community engagement with home visits intensified in Dolisie has been implemented, including hygiene promotion activities.
- The MSP has strengthened clinical care capacity by deploying additional surgeons to operate on patients with perforations and developing a care plan based on antibiotic susceptibility patterns.
WHO risk assessment
Although no epidemiological baseline data is available for previous years, the high number of suspected cases and deaths of suspected typhoid fever and Shigella reported within two months, led to an overflow of health facilities as well as the high number of patients reported that have undergone surgical intervention due to intestinal perforation, are considered unusual.
Although sporadic cholera outbreaks have been reported in the Republic of Congo, the city of Dolisie, the current epicentre, has not previously recorded such an outbreak. Cholera outbreaks are ongoing in the neighbouring countries of the Democratic Republic of the Congo and Cameroon, but no epidemiolocal link has been identified. So far, no disease spread to other countries has been reported linked to this outbreak.
WHO assesses the risk at the national level as high. This is based on the rapid outbreak dynamic and high morbidity and mortality of this outbreak, the strain on the health care system and high risk of healthcare–associated infections, the limited access to safe drinking water in Dolisie, the poor water and sanitation infrastructure, poor hygiene practices, and the observed limitations in the rapid detection, confirmation, and management of suspected cases. The limited information available on laboratory confirmations and implicated antimicrobial resistance (AMR) profiles further complicates the tailoring of an effective public health response. Regional and global levels of risk are considered moderate and low, respectively.
WHO advice
The outbreak highlights the importance of public health measures to prevent the spread of resistant and non-resistant pathogens. Since this outbreak involves multiple Gram-negative bacteria, special attention should be paid to the possible presence of extended-spectrum beta-lactamases (ESBLs) and carbapenemases, as they can spread horizontally between species and further complicate treatment. Additionally, although S. typhi isolates are reported to be susceptible to ciprofloxacin, reported resistance to nalidixic acid might indicate reduced susceptibility to fluoroquinolones.
While emerging resistance in S. typhi would indeed complicate treatment, typhoid fever remains common in places with poor sanitation and a lack of safe drinking water. Access to safe water and adequate sanitation, hygiene among food handlers and typhoid vaccination are the main and most important recommendations. WHO recommends typhoid vaccination in response to confirmed outbreaks of typhoid fever and recommends vaccination should be considered for travellers to typhoid-endemic areas. Further, where the typhoid conjugate vaccine (TCV) is licensed, WHO recommends TCV (among the available typhoid vaccines) as the preferred vaccine in view of its improved immunological properties. Typhoid vaccination should be implemented in the context of other efforts to control the disease. Also, seeing how quickly S. typhi can acquire new resistance mechanisms, WHO recommends strengthening surveillance of antimicrobial resistance to monitor known resistance, detect new and emerging resistance, control its spread and share the surveillance data locally and internationally in a timely manner.
For surveillance, prompt detection and reporting of cases of bloody diarrhoea is the essential first step to monitoring endemic shigellosis and controlling epidemic shigellosis. Laboratory surveillance should be used to isolate and identify Shigella and perform antimicrobial susceptibility testing. State Parties are encouraged to refer to WHO guidance documents on foodborne disease surveillance and response.
WHO recommends improving access to clean water and sanitation to prevent cholera transmission. Strengthening surveillance, especially at the community level, is advised. Appropriate case management, including improving access to care by establishing cholera treatment centers and oral rehydration points in the community, should be implemented in outbreak-affected areas to reduce mortality. Oral cholera vaccines (OCV) should be used in conjunction with improved water and sanitation to control cholera outbreaks and for prevention in areas known to be at high risk for cholera. It is necessary to ensure that countries are prepared to quickly detect and respond to any cholera outbreak to reduce the risk of it spreading to new areas.
WHO recommends infection prevention and control, water, sanitation, and hygiene, waste management and food safety practices at health facilities be closely monitored and improved where gaps are identified, particularly for facilities experiencing surges of patients. Contact precautions, including isolation of cases, should be enabled in health facilities for all patients who present with acute onset of gastroenteric symptoms, particularly for those experiencing incontinence. Efforts should be made to avoid cohort isolation of patients with different gastroenteric infections. Health facilities should closely monitor for instances where inpatients who are admitted for other reasons develop symptoms of gastroenteric infection beyond 48 hours admission as an inpatient, as this is indicative of potential healthcare-associated infection.
WHO advises against applying any travel or trade restrictions based on the current information available on this event.
Further information
- Ministère de la Santé et de la Population Congo. Declaration des epidemies de cholera, shigellose et fievre typhoide dans la ville de dolisie, département du niari.
- WHO fact sheets – Typhoid
- WHO Guidelines for the control of shigellosis, including epidemics due to Shigella dysenteriae type1
- WHO fact sheets – Cholera
- Multi-country outbreak of cholera, External situation report #6 – 6 September 2023
- Global Task Force on Cholera Control
- Technical Guidelines for Integrated Disease Surveillance and Response in the African Region: Third edition
Citable reference: World Health Organization (21 September 2023). Disease Outbreak News; Suspected triple outbreak of typhoid fever, shigellosis and cholera – Congo. Available at: https://www.who.int/emergencies/disease-outbreak-news/item/2023-DON488