In a groundbreaking study, researchers from the University of Leicester have discovered that tuberculosis (TB) disrupts glucose metabolism in the body, which could promote the onset of metabolic diseases like diabetes. The findings, published in PLoS Pathogens, highlight the possibility that undiagnosed or subclinical TB may push vulnerable individuals toward metabolic conditions, offering a new perspective on the intricate relationship between TB and diabetes.
Tuberculosis, a bacterial infection primarily affecting the lungs, is one of the deadliest infectious diseases globally, causing over 4,000 deaths each day. While TB primarily compromises respiratory function, its effects on other organs, including the liver, have now come under closer scrutiny. Scientists at the University of Leicester’s Tuberculosis Research Group have been focusing on how TB impacts liver metabolism, particularly in undiagnosed cases.
The study’s co-author, Professor Andrea Cooper, explained the importance of this discovery: “Our paper shifts the focus from diabetes worsening TB to the possibility that late diagnosis of TB disrupts glucose metabolism, potentially leading to insulin resistance and the progression to diabetes in susceptible individuals.” This revelation underscores the potential for undiagnosed TB to act as a precursor to metabolic diseases, particularly in populations with compromised immune systems or pre-existing health conditions.
A New Perspective on TB’s Systemic Impact
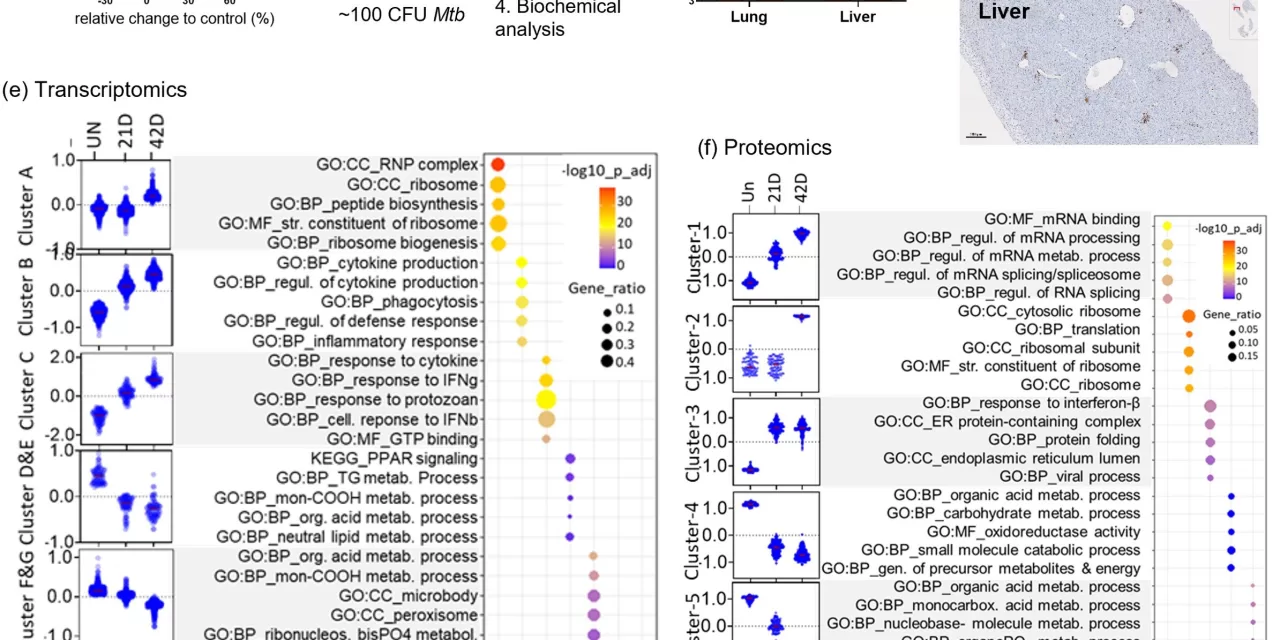
The research team used laboratory models of pulmonary TB to investigate early changes in liver function. They discovered that TB triggers an immune response in the liver cells, altering glucose metabolism. This immune response not only affects how the liver processes glucose but also influences insulin sensitivity, potentially setting the stage for the development of diabetes.
Further analysis by Dr. Mrinal Das, the study’s primary author, re-examined metabolic data from human cases of TB. Das found that disruptions in liver glucose metabolism were evident in patients who transitioned from latent TB (where the infection is present but asymptomatic) to active disease. This finding reinforces the theory that even latent TB infections could negatively impact metabolic health.
Implications for Future TB Treatment and Diabetes Management
The discovery that TB can alter glucose metabolism has significant implications for both the treatment of TB and the management of diabetes. Diabetes has long been known to exacerbate TB outcomes, complicating the effectiveness of drug treatments. However, this study adds a new layer to the understanding, suggesting that TB itself may contribute to the onset of diabetes, particularly in individuals with undiagnosed infections.
“As diabetes compromises drug treatment, our paper supports the idea that metabolic screening should be integrated into drug and vaccine trials for TB,” Professor Cooper emphasized. By identifying and addressing disruptions in glucose metabolism early, healthcare providers may be able to mitigate the dual burden of TB and diabetes in vulnerable populations.
Looking Forward: Targeted Interventions and Vaccine Development
One of the key goals of the research team moving forward is to define the molecular pathways through which TB-induced immune responses alter liver metabolism. “Our future aim is to create targeted interventions that could address these metabolic disruptions,” Professor Cooper added. The team also plans to investigate the broader impacts of latent TB on human metabolic health, potentially paving the way for new therapeutic strategies that could help prevent the progression of both TB and diabetes.
This discovery also adds urgency to global efforts to improve TB vaccination. Currently, only one vaccine exists for TB, primarily used in infants and young children. With the emergence of new data linking TB to metabolic diseases, there is a growing need for better diagnostic tools and preventive measures that account for the systemic impacts of TB, particularly in adults.
The study’s insights offer hope for more comprehensive approaches to TB treatment, which could alleviate the dual threats of tuberculosis and diabetes.
For more information, refer to the original study: Mrinal K. Das et al, “Altered hepatic metabolic landscape and insulin sensitivity in response to pulmonary tuberculosis,” published in PLOS Pathogens (2024).
This article highlights the broader implications of the University of Leicester’s research findings, connecting the dots between infectious diseases like TB and non-communicable conditions such as diabetes. The study paves the way for further exploration into metabolic health, offering hope for improved treatments and prevention strategies.