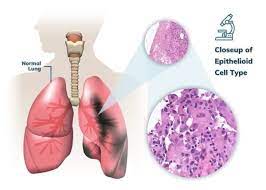
Researchers have discovered that analyzing the volatile organic chemicals present in the exhaled breath of individuals afflicted with malignant pleural mesothelioma (MPM) holds potential as a screening tool for the disease. MPM, a challenging condition with limited curative options and a grim prognosis, has prompted scientists to seek predictive markers that could improve treatment outcomes and personalize medicine for individual patients. Recently, volatile organic molecules (VOCs) in exhaled breath have garnered attention as possible non-invasive indicators of the disease.
Kevin Lamote, PhD, along with colleagues from the University of Antwerp in Belgium, conducted a study utilizing VOCs as predictive biomarkers. They aimed to determine if exhaled breath analysis could differentiate between treatment responders and non-responders (discriminative setup) and, if successful, forecast treatment outcomes in advance (predictive setup). Dr. Lamote and his team evaluated 13 MPM patients, subjecting them to CT scans both before and every three months post-therapy, with results categorized as stable (SD) or progressive (PD) based on mRECIST standards. Multicapillary column-ion mobility spectrometry (MCC-IMS) was employed to collect breath samples and background samples from the patients at each time point, in order to characterize VOCs. A lasso regression was conducted to identify VOCs capable of distinguishing between responders and non-responders post-treatment. Additionally, using previously gathered breath samples, a predictive model was developed to anticipate treatment outcomes.
The study reported an 89 percent accuracy in identifying SD and PD patients during follow-up. Encouragingly, the predictive model was able to forecast treatment results with the same level of accuracy from the outset. Notably, no discernible differences in treatment response were observed between SD and PD patients, suggesting that the selected VOCs may not be treatment-specific but could be implicated in broader mechanisms or associated with the tumor microenvironment.
Dr. Lamote remarked, “The identification of VOCs in exhaled breath represents a promising opportunity for non-invasive detection and prediction of treatment outcomes in MPM patients.” He further emphasized the need for larger population studies to validate the utility of the VOC profile. Additionally, fine-tuning the VOC profile for each treatment could assist in predicting which patients are most likely to benefit from specific therapies, ultimately leading to improved overall treatment regimens for MPM.









