A groundbreaking study suggests that incorporating sex-specific criteria into machine learning models could revolutionize the diagnosis and treatment outcomes of cardiovascular disease (CVD) in women, an area long plagued by underdiagnosis compared to men.
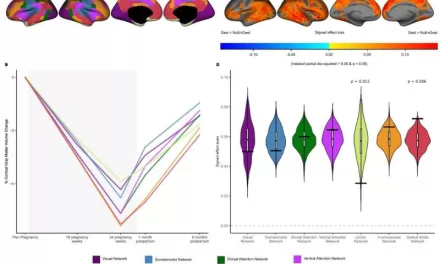
Published in the journal Frontiers in Physiology, the research underscores the critical need for tailored diagnostic approaches, considering anatomical disparities between male and female hearts. Despite women having smaller hearts with thinner walls, diagnostic criteria for certain heart diseases have traditionally remained uniform across genders.
“This one-size-fits-all approach results in a significant underdiagnosis of cardiovascular disease in women, particularly in cases of first-degree atrioventricular block and dilated cardiomyopathy,” stated researchers in the paper, led by Skyler St Pierre from Stanford University’s Living Matter Lab in the US.
The study revealed that relying on sex-neutral criteria leads to women’s underdiagnosis being twice as severe in cases of first-degree atrioventricular block and 1.4 times more severe in cases of dilated cardiomyopathy compared to men.
“To address this disparity, we propose integrating sex-specific criteria into diagnostic models, which would mitigate the underdiagnosis observed in women,” St Pierre explained.
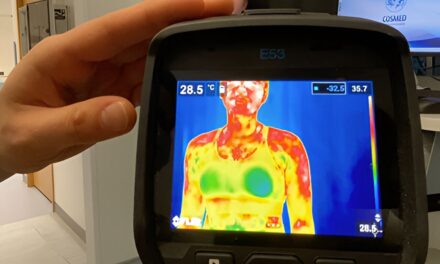
The researchers advocated for the integration of additional metrics, including cardiac magnetic resonance imaging, pulse wave analysis, electrocardiograms (EKGs), and carotid ultrasounds, to enhance the accuracy of heart risk models.
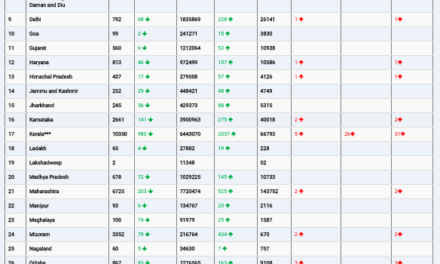
In their analysis of data from over 20,000 individuals in the UK Biobank database, the team identified EKGs as the most effective tool for improving the detection of CVD in both men and women. However, they emphasized that traditional risk factors such as age, sex, cholesterol levels, and blood pressure remain vital components of risk assessment.
“We suggest a two-stage screening approach, where individuals are initially evaluated using a basic survey encompassing traditional risk factors, followed by a secondary screening involving EKGs for high-risk patients,” the researchers concluded.
By leveraging advanced machine learning techniques and embracing sex-specific criteria, healthcare professionals may soon achieve more accurate diagnoses and tailored treatment strategies, thereby addressing longstanding disparities in cardiovascular care for women.