A groundbreaking analysis encompassing over 13,000 individuals has unearthed significant alterations in brain blood vessels that could heighten the risk of stroke and dementia in patients with various heart conditions, irrespective of their stroke history.
Published today in Neurology®, the esteemed medical journal of the American Academy of Neurology, the research marks the most extensive systematic review to date of concealed brain changes in individuals grappling with a spectrum of heart ailments.
Lead author Dr. Zien Zhou from The George Institute for Global Health underscores the paramount importance of identifying these changes in guiding treatment decisions for affected patients. Dr. Zhou emphasizes that individuals with heart disease, although at a heightened risk of brain vascular system alterations, often elude detection due to the absence of routine brain imaging unless a stroke has occurred.
Dr. Zhou elucidates, “Unveiling these covert cerebrovascular changes assumes critical significance as they render patients more susceptible to the peril of brain bleeds stemming from medications commonly employed to treat or prevent blood clots.”
These concealed changes, detectable solely through brain imaging, encompass silent brain infarction (SBI) and cerebral small vessel disease (CSVD), prevalent among older individuals or those grappling with hypertension. Although devoid of overt neurological symptoms, these changes can precipitate subtle neurological deficits and escalate the long-term susceptibility to stroke or dementia.
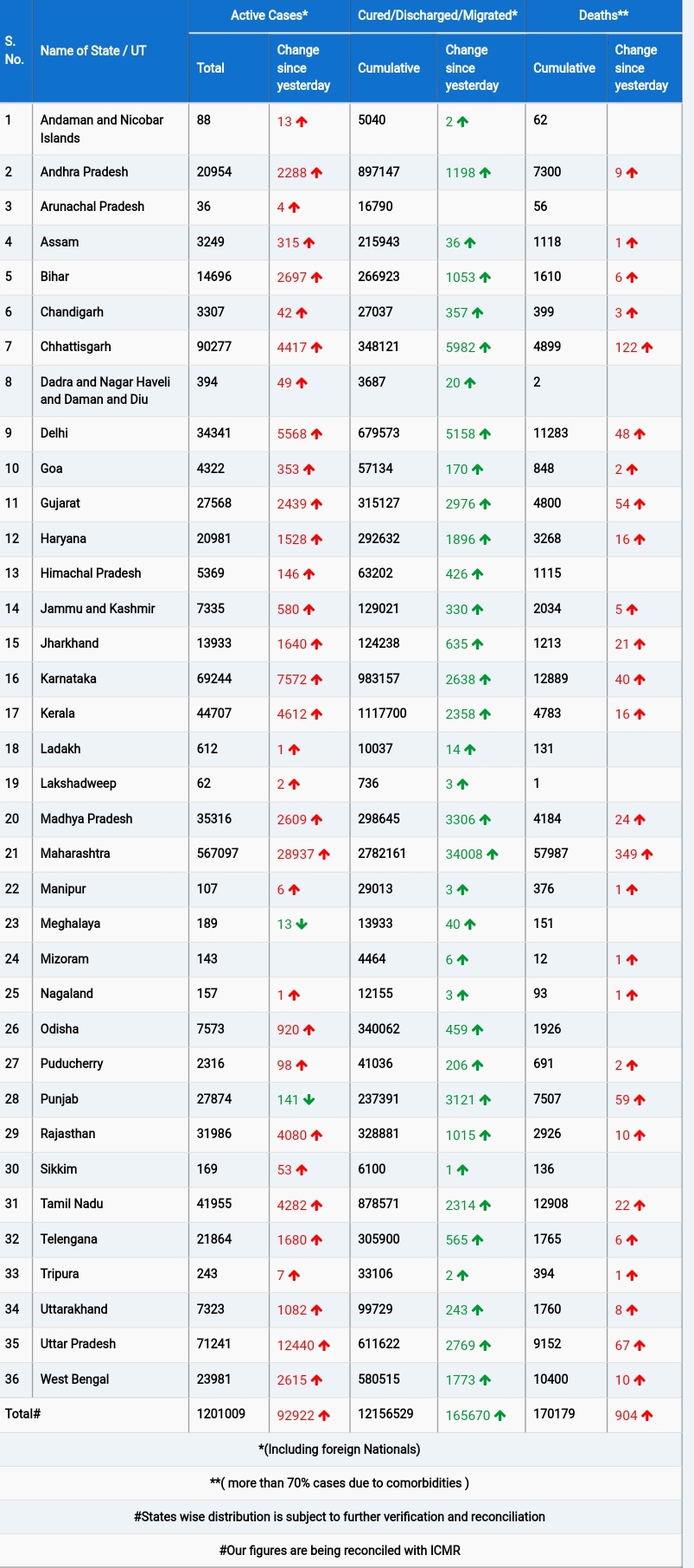
To ascertain the prevalence of these obscured cerebrovascular changes across various heart conditions, researchers from The George Institute conducted a meta-analysis of 221 observational studies spanning from 1988 to 2022. The analysis encompassed individuals grappling with atrial fibrillation, coronary artery disease, heart failure or cardiomyopathy, heart valve disease, and patent foramen ovale.
The findings unveiled a significant prevalence of concealed brain changes among heart disease patients, including SBI, lacune, white matter lesions, asymptomatic microbleeds, and brain atrophy. Surprisingly, the prevalence remained consistent irrespective of recent stroke occurrence, with no discernible sex differences.
Dr. Zhou emphasizes, “Heart disease emerges as a primary instigator of these changes, reflecting brain ‘frailty,’ with common risk factors such as ageing, hypertension, type 2 diabetes, hyperlipidaemia, and smoking exacerbating the condition.”
While proposing several potential mechanisms underlying the association between heart disease and concealed cerebrovascular injury, Dr. Zhou underscores the imperative of further research to unravel the exact causes and management implications.
He concludes, “Refining the risks associated with brain clots and bleeds from anticoagulants and leveraging this information to tailor treatment strategies could significantly enhance treatment safety for individuals grappling with heart disease.”
This groundbreaking study sheds new light on the intricate interplay between heart conditions and hidden brain changes, offering a promising avenue for optimizing treatment modalities and enhancing patient outcomes.