Philadelphia, PA – A groundbreaking study by researchers from the Mitochondrial Medicine Program at Children’s Hospital of Philadelphia (CHOP) has shed new light on mitochondrial DNA deletion syndromes, revealing a broader spectrum of disease progression than previously understood. Published today in Genetics in Medicine, the study enhances our understanding of these disorders and may influence future clinical trials.
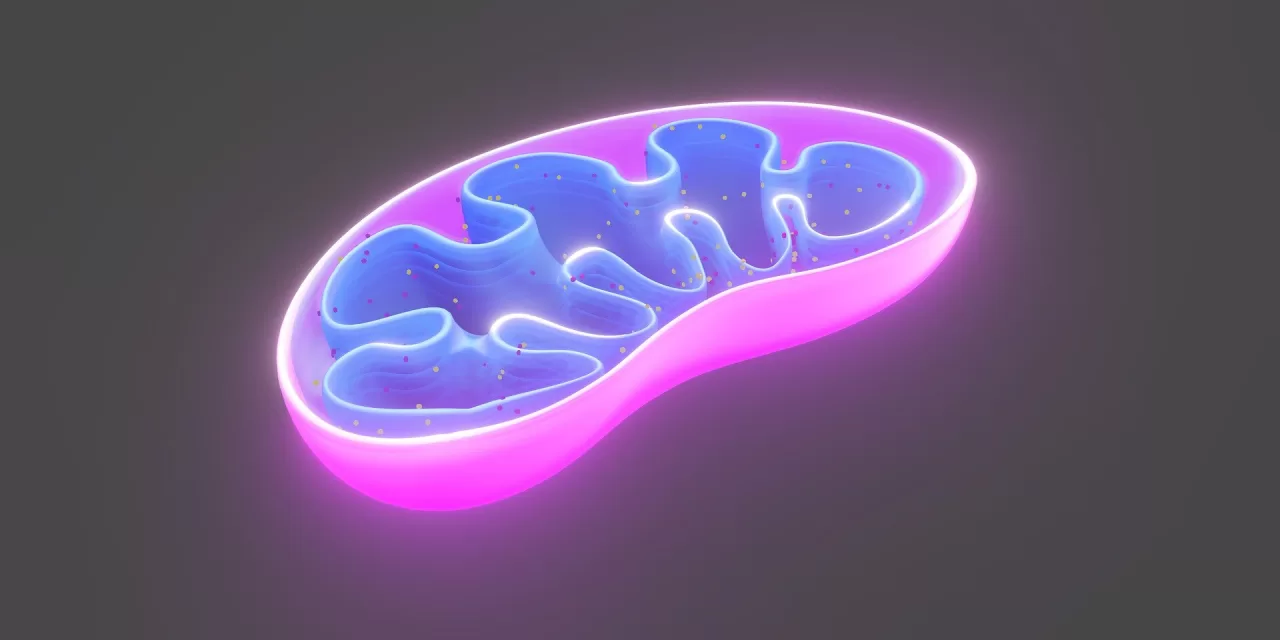
Mitochondrial diseases encompass a range of disorders affecting mitochondria, the cellular powerhouses responsible for energy production. Among these, Pearson syndrome, Kearns-Sayre syndrome (KSS), and chronic progressive external ophthalmoplegia (CPEO) are each caused by single large-scale mitochondrial DNA (mtDNA) deletions (SLSMD), which involve significant loss of genetic material within the mitochondria.
Despite their shared genetic root, these syndromes manifest differently: Pearson syndrome typically emerges in infancy with symptoms like anemia and growth failure; KSS presents in childhood with progressive multi-system effects; and CPEO often appears in adulthood, primarily impacting eye muscle movement. The study aimed to refine the clinical understanding of SLSMD syndromes by analyzing 30 cases documented at CHOP between 2002 and 2020.
Expanding the Clinical Spectrum
Dr. Rebecca Ganetzky, first author of the study and attending physician in Mitochondrial Medicine at CHOP, emphasized that while these three conditions represent the named syndromes, the spectrum of SLSMD disorders extends beyond them. “Many patients exhibit symptoms that do not fit within strict diagnostic criteria,” she noted. This expanded understanding may allow future clinical trials to include a wider range of patients, leading to more comprehensive evaluations of disease progression and quality-of-life impacts.
One of the key findings was the recurrent deletion within the gene MT-ND5, observed in 96% of SLSMD patients, regardless of their clinical presentation. Additionally, the biomarker peptide growth differentiation factor 15 (GDF-15) was consistently elevated among patients, suggesting potential diagnostic and prognostic applications.
Implications for Future Research
The study also uncovered a correlation between higher levels of SLSMD heteroplasmy—a phenomenon in which both normal and deleted mtDNA coexist in a patient—and earlier disease onset. As patients aged, fatigue levels increased while quality of life declined.
Senior author Dr. Marni Falk, Executive Director of the Mitochondrial Medicine Program at CHOP, highlighted the study’s innovative approach, stating, “This research demonstrates how retrospective clinical data analysis can effectively define the natural history of rare diseases, accelerating our ability to develop targeted treatments.”
The findings hold promise for refining clinical trial criteria and potentially developing new therapeutic strategies. As the field of genetic therapies continues to advance, studies like this pave the way for a more nuanced and responsive approach to treating rare mitochondrial disorders.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Readers are encouraged to consult healthcare professionals for personalized medical guidance.