In a groundbreaking study, researchers from Lund University in Sweden have discovered that defects in sperm are significantly linked to an increased risk of preeclampsia in pregnancies achieved through in vitro fertilization (IVF). The study, published in Fertility and Sterility, marks the first time that specific defects in sperm have been directly connected to pregnancy complications and adverse health outcomes for newborns.
The research reveals that when a high percentage of the father’s sperm carries DNA strand breaks, the risk of the mother developing preeclampsia is doubled. Preeclampsia, a serious condition that affects pregnant women and can lead to premature birth, is a leading cause of maternal and neonatal morbidity and mortality worldwide. The findings also indicate a higher risk of premature birth in such pregnancies.
Unveiling a Hidden Cause of Pregnancy Complications
Although it has long been recognized that pregnancies achieved through assisted reproduction techniques (ART) come with heightened risks—such as preeclampsia, miscarriage, and premature birth—the precise reasons for these risks have remained elusive. This new study, however, sheds light on a previously underexplored factor: the quality of the father’s sperm.
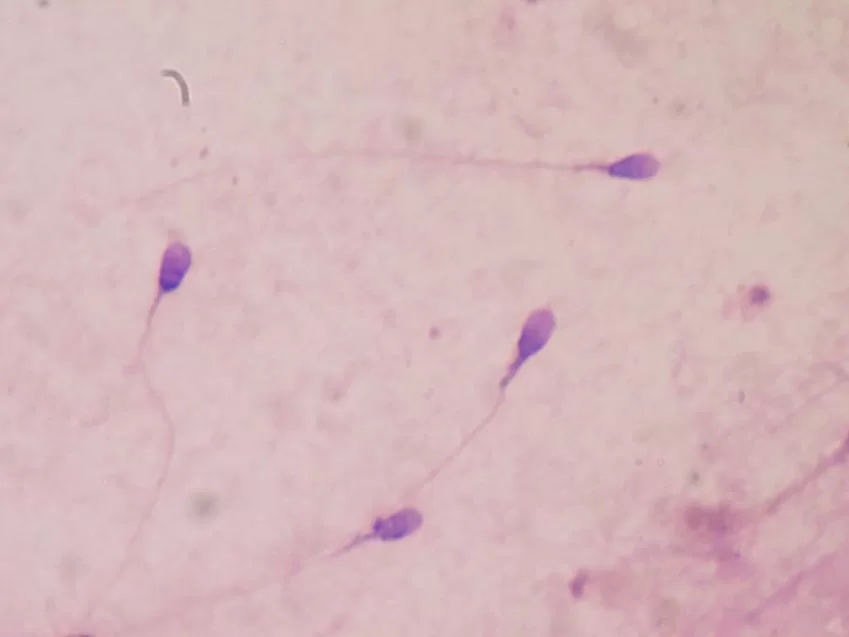
Dr. Amelie Stenqvist, a lecturer at Lund University and specialist in gynecology and obstetrics at Skåne University Hospital, explains that current sperm analysis techniques used before IVF procedures often fail to detect DNA fragmentation. “There are men who, according to standard analyses, have normal sperm but still experience reduced fertility,” Stenqvist notes. DNA fragmentation, measured using the DNA Fragmentation Index (DFI), can reveal damage not captured by conventional sperm tests, which typically assess concentration, motility, and morphology.
Around 20–30% of babies born through IVF have fathers with elevated DNA fragmentation levels. A high DFI—above 30%—dramatically reduces the likelihood of natural conception.
Linking Sperm DNA Damage to Preeclampsia
To explore how sperm DNA damage might influence pregnancy outcomes, a research team led by Professor Aleksander Giwercman, a specialist in reproductive medicine at Lund University, analyzed data from 1,660 children conceived via IVF and intracytoplasmic sperm injection (ICSI) between 2007 and 2018. The study found that in IVF pregnancies, if the father’s sperm had a DFI over 20%, the risk of preeclampsia more than doubled to 10.5%. This rate stands in contrast to a 4.8% preeclampsia risk in pregnancies where the sperm DFI was below 20%, a figure comparable to natural conceptions.
Interestingly, the study noted no increased risk of preeclampsia in pregnancies achieved via ICSI, a procedure in which a single sperm is injected directly into the egg.
A Call for Standardized DFI Testing
Currently, DFI analysis is not standard practice at fertility clinics in Sweden. The study’s authors argue that this should change. “We believe DFI analysis should be introduced as a routine test at all fertility clinics,” says Giwercman. Such testing could help identify couples struggling with unexplained infertility and offer insight into potential pregnancy risks.
The research also highlights the broader implications of sperm DNA fragmentation. Factors such as oxidative stress, smoking, obesity, aging, and infections contribute to DNA damage. This opens the door to potential interventions, including lifestyle modifications, to improve sperm quality and reduce pregnancy complications.
“The next step is to identify which men respond best to treatments aimed at reducing sperm DNA damage and to test whether these treatments can help prevent complications like preeclampsia,” adds Stenqvist.
The findings could revolutionize both infertility treatment and prenatal care, offering new tools to enhance pregnancy outcomes for couples undergoing assisted reproduction.
Journal Reference:
Amelie Stenqvist et al. High sperm deoxyribonucleic acid fragmentation index is associated with an increased risk of preeclampsia following assisted reproduction treatment, Fertility and Sterility (2024). DOI: 10.1016/j.fertnstert.2024.08.316