Date: January 1, 2025
A groundbreaking study from the Children’s Medical Center Research Institute (CRI) at UT Southwestern has revealed a disturbing link between certain beta-blockers and higher mortality rates following hematopoietic cell transplants, commonly used to treat blood cancers like leukemia. Published in Cancer Discovery, the research highlights how the use of non-selective beta-blockers during this critical treatment may impair the regeneration of bone marrow, leading to potentially life-threatening complications.
The study, led by Dr. Sean J. Morrison, Director of CRI and Howard Hughes Medical Institute Investigator, provides compelling evidence that beta-blockers—specifically non-selective ones—can significantly delay bone marrow regeneration in patients undergoing hematopoietic cell transplants. This delay in recovery can result in prolonged vulnerability to infections and complications, ultimately increasing the risk of death.
“We believe this discovery has the potential to save lives by improving how we manage patients undergoing hematopoietic cell transplants,” said Dr. Morrison. “Our findings could drastically change treatment protocols for these vulnerable patients.”
The Science Behind the Discovery
Hematopoietic cell transplants are used to treat disorders of the blood-forming system, such as high-risk leukemia. During these procedures, a patient’s blood-forming cells are destroyed through chemotherapy and radiation, then replaced with healthy stem cells from a donor. These transplanted cells help regenerate the patient’s blood-forming system, but the process leaves the patient vulnerable for weeks until their blood cell counts recover.
In earlier research, Dr. Morrison and his team discovered that nerves play a crucial role in bone marrow regeneration by activating β2 and β3 adrenergic receptors in the hematopoietic stem cell niche. These receptors, which are targeted by beta-blockers, are essential for the repair of bone marrow after treatments like chemotherapy.
Beta-Blockers and Bone Marrow Regeneration
Beta-blockers, particularly non-selective ones, inhibit signaling through all three beta-adrenergic receptors (β1, β2, and β3). These medications, which are commonly used to treat conditions like high blood pressure and cardiovascular diseases, may impair the bone marrow’s ability to regenerate by blocking crucial nerve signals.
To investigate this further, CRI scientists tested the hypothesis in mouse models, confirming that non-selective beta-blockers indeed delayed bone marrow regeneration in transplanted mice. In fact, half of the mice treated with non-selective beta-blockers died due to insufficient bone marrow recovery, underscoring the severity of the issue.
Implications for Human Patients
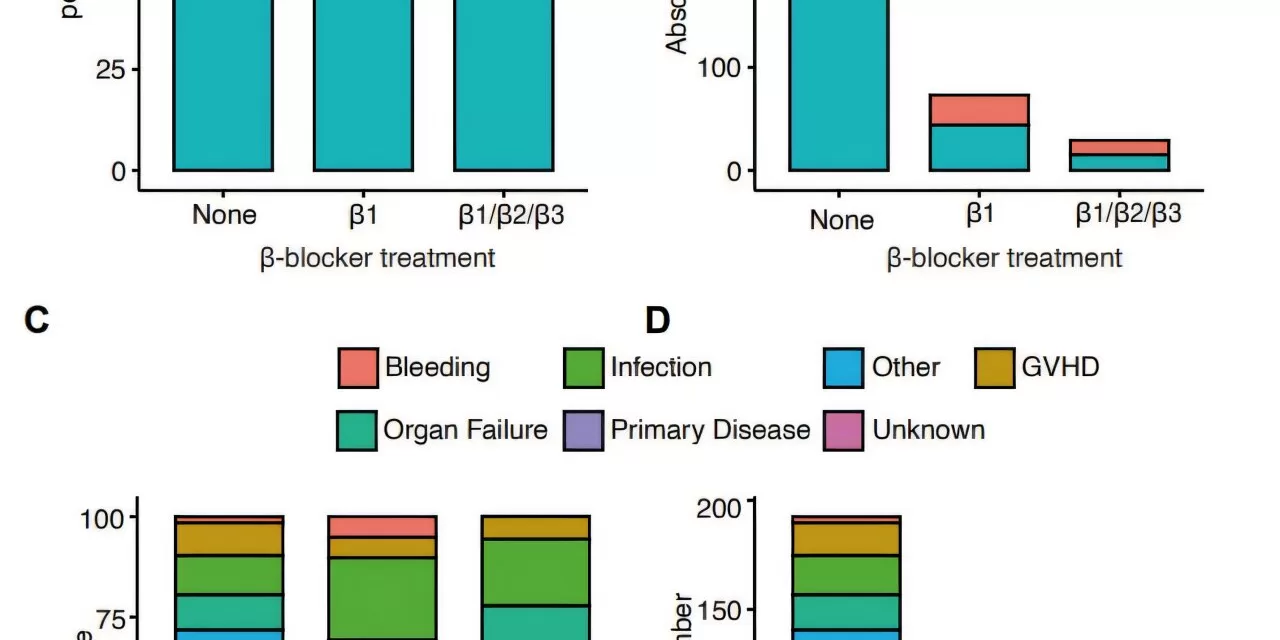
To assess the relevance of these findings in human patients, Dr. Morrison collaborated with Dr. Stephen Chung, Assistant Professor of Internal Medicine at CRI, and Dr. Ashwin Kishtagari, Assistant Professor of Medicine at Vanderbilt University. They analyzed retrospective data from patient cohorts who had received allogeneic (unrelated donor) hematopoietic cell transplants at their respective institutions.
The data revealed that patients who continued to take non-selective beta-blockers post-transplant experienced significantly delayed blood count recovery, leading to a higher incidence of complications and poorer survival outcomes. Dr. Chung emphasized the importance of these findings for blood cancer patients, who typically remain hospitalized for weeks until their blood counts stabilize after the transplant.
Potential Clinical Changes
The study’s results could lead to significant changes in clinical practice, especially in how beta-blocker use is managed during hematopoietic cell transplants. Dr. Kishtagari suggested that patients either discontinue non-selective beta-blockers for at least three weeks after the transplant or switch to β1-selective inhibitors if discontinuation is not an option.
While the study’s findings are compelling, the researchers caution that further confirmation in additional patient cohorts is necessary, given the variability in transplant protocols across medical institutions.
Conclusion
This study sheds new light on the critical role of beta-adrenergic signaling in bone marrow regeneration and its impact on the success of hematopoietic cell transplants. As scientists continue to explore how medications affect the recovery process, it is clear that understanding and adjusting the use of beta-blockers could have life-saving implications for patients undergoing these high-risk procedures.
For more information, the full study is available in Cancer Discovery (DOI: 10.1158/2159-8290.CD-24-0719).