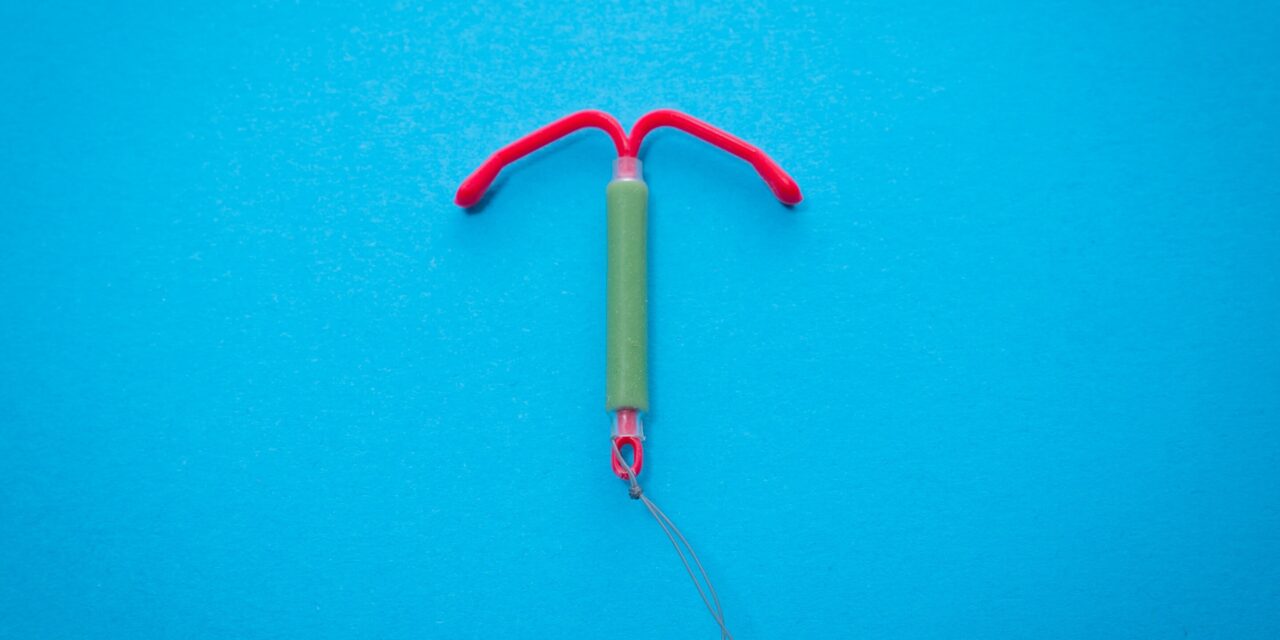
A recent study published in the Journal of the National Cancer Institute by researchers from the University of Queensland and the QIMR Berghofer Medical Research Institute has revealed that long-acting contraceptives—such as intrauterine devices (IUDs), implants, and injections—pose a cancer risk comparable to that of the oral contraceptive pill. The study sheds light on the cancer-related concerns surrounding hormonal contraception and provides reassurance for women who use these methods for birth control.
Hormonal Contraceptives and Cancer Risk
Concerns about the potential for hormonal contraceptives to increase cancer risk have long been a topic of discussion. While the International Agency for Research on Cancer has acknowledged the mixed effects of the oral contraceptive pill on cancer risk, the evidence is more nuanced than often perceived.
The oral contraceptive pill has been linked to a slight increase in breast and cervical cancer risk in the short term, but it is also known to significantly reduce the risk of uterine and ovarian cancers over the long term. Previous studies have shown that in Australia, the pill prevented over 1,300 cases of endometrial and ovarian cancers in 2010 alone, along with nearly 500 cancer-related deaths in 2013.
Long-Acting Reversible Contraceptives (LARCs) and Cancer Risk
Long-acting reversible contraceptives (LARCs), which include hormone-releasing IUDs, implants, and injections, have gained popularity in recent years. These contraceptives, unlike the pill, do not contain estrogen—one of the hormones believed to contribute to some of the pill’s side effects, including a potential higher risk of breast cancer.
The recent study, which examined over 1 million Australian women, compared cancer rates among users of LARCs and oral contraceptive pills. The findings suggest that LARCs carry a similar cancer risk profile to that of the pill, with the added benefit of not containing estrogen.
Findings on Cancer Risks
The study found that long-term use of hormonal contraception, whether from the pill or LARCs, significantly reduces the risk of endometrial and ovarian cancers. Specifically, users of hormonal contraception were shown to have a 70% lower risk of developing endometrial cancer and a 50% lower risk of ovarian cancer compared to women who did not use hormonal contraception.
While the risk of breast cancer for current users of LARCs was similar to that of the pill, the study noted that the contraceptive injection was associated with a slight increase in breast cancer risk after five years of use. However, once women stopped using the injection, the elevated risk appeared to subside. This reduction in risk was also observed for implant users.
No Significant Link to Other Cancers
The study did not show a consistent relationship between hormonal contraceptive use and other types of cancer, such as lung or colorectal cancer. However, the researchers did highlight a French study that suggested a small increased risk of meningioma (a benign brain tumor) for prolonged use of the contraceptive injection, though meningiomas are extremely rare in women under 40.
A Balanced Approach to Contraception
Despite the concerns around cancer, the researchers emphasize that the risks associated with hormonal contraceptives are very small. For example, the incidence of breast cancer among women aged 20 to 39 is about 30 cases per 100,000 each year. Using hormonal contraceptives might increase that rate slightly, to around 36 cases per 100,000.
While there are potential side effects to consider, most serious complications are rare. The researchers encourage women to have open conversations with their healthcare providers to weigh the benefits and risks of different contraceptive methods based on individual health profiles and family history.
Conclusion
This study offers reassuring news for women considering hormonal contraceptives, whether the pill or long-acting alternatives. It confirms that these methods, when used appropriately, carry a minimal and manageable cancer risk—providing women with more options for family planning and peace of mind regarding their health.
For those interested in the full study, it was published in the Journal of the National Cancer Institute.
Source: Journal of the National Cancer Institute, University of Queensland, QIMR Berghofer Medical Research Institute