A recent modeling study has concluded that offering the HPV vaccination to adults aged 27 to 45 is unlikely to be cost-effective, with the benefits being significantly lower compared to vaccinating younger individuals. The findings, published in the Annals of Internal Medicine, are the result of a study that evaluated the cost-effectiveness of expanding the current HPV vaccination program, which is typically offered to individuals aged 9-26, to include adults in the 27-45 age range.
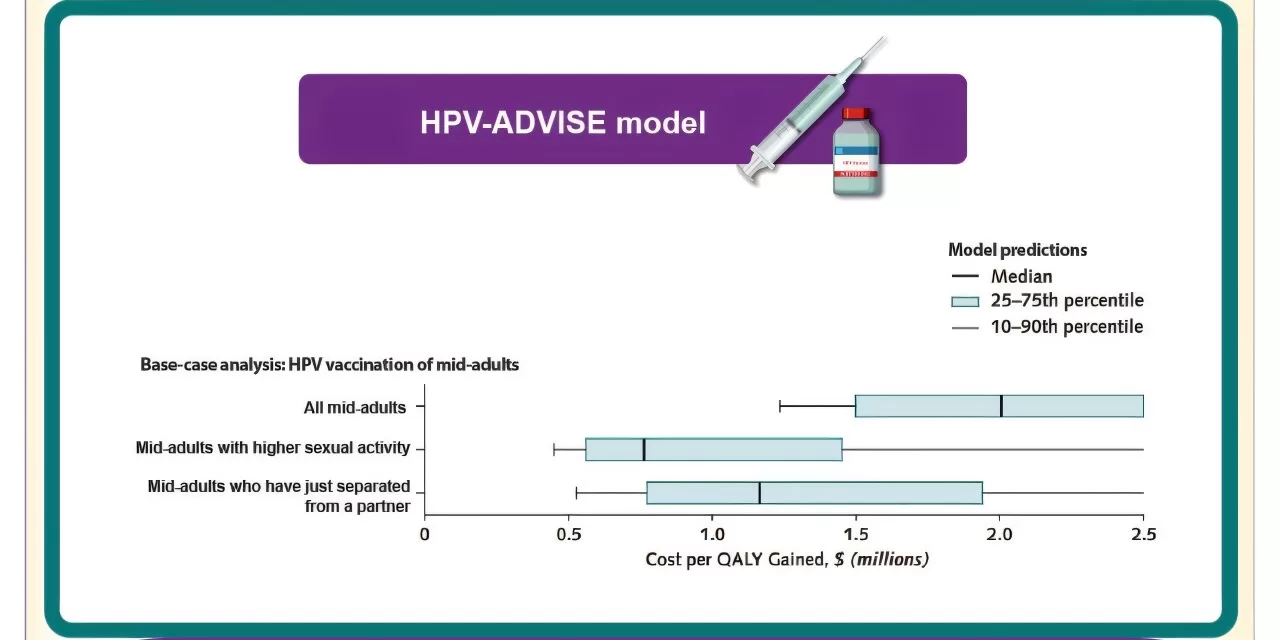
In June 2019, the US Advisory Committee on Immunization Practices (ACIP) recommended that HPV vaccination for adults aged 27 to 45 be considered on a case-by-case basis, allowing shared clinical decision-making between doctors and patients. To assess the effectiveness of such a strategy, researchers from Laval University in Quebec City used a computer model to simulate various scenarios. They focused on adults in this age group with a higher risk of HPV infection, including those with higher sexual activity or individuals who had recently separated from long-term intimate partners.
The study’s results were clear: under all scenarios tested, vaccinating adults aged 27-45 was far less cost-effective than vaccinating individuals aged 26 or younger. The number of people who would need to be vaccinated (NNV) to prevent a single case of HPV-related cancer was considerably higher in the older group, making the approach more expensive and less efficient.
However, the researchers did identify a subgroup where the extension of the HPV vaccination could be more cost-effective: mid-adult women who have infrequent screening, a history of higher sexual activity, and who have recently separated from a long-term partner. For this group, the study found that the cost-effectiveness and the NNV were notably lower than for other subgroups within the 27-45 age range.
Despite these findings, the study emphasized that vaccinating younger people—those aged 26 and younger—remains a far more cost-effective and effective approach to preventing HPV-related cancers. The authors suggest that while extending vaccination to older individuals could be beneficial for certain high-risk groups, the overall public health impact would be less significant than focusing on younger populations.
This study is the first to specifically examine the cost-effectiveness of targeting subgroups of adults aged 27 to 45 years for HPV vaccination, providing valuable insight into how vaccination strategies could be optimized.
For more information, the full study is available in the Annals of Internal Medicine.
Jean-François Laprise et al, “Cost-Effectiveness of Extending Human Papillomavirus Vaccination to Population Subgroups Older Than 26 Years Who Are at Higher Risk for Human Papillomavirus Infection in the United States,” Annals of Internal Medicine (2024). DOI: 10.7326/M24-0421