SAN FRANCISCO, CA – A new study presented at the 2025 Conference on Retroviruses and Opportunistic Infections (CROI) has examined the effectiveness of mobile health units in providing integrated addiction and HIV care to individuals who inject drugs. Researchers from the HIV Prevention Trials Network (HPTN) presented the results of the HPTN 094 (“INTEGRA”) study, a randomized controlled trial designed to assess the impact of this novel approach.
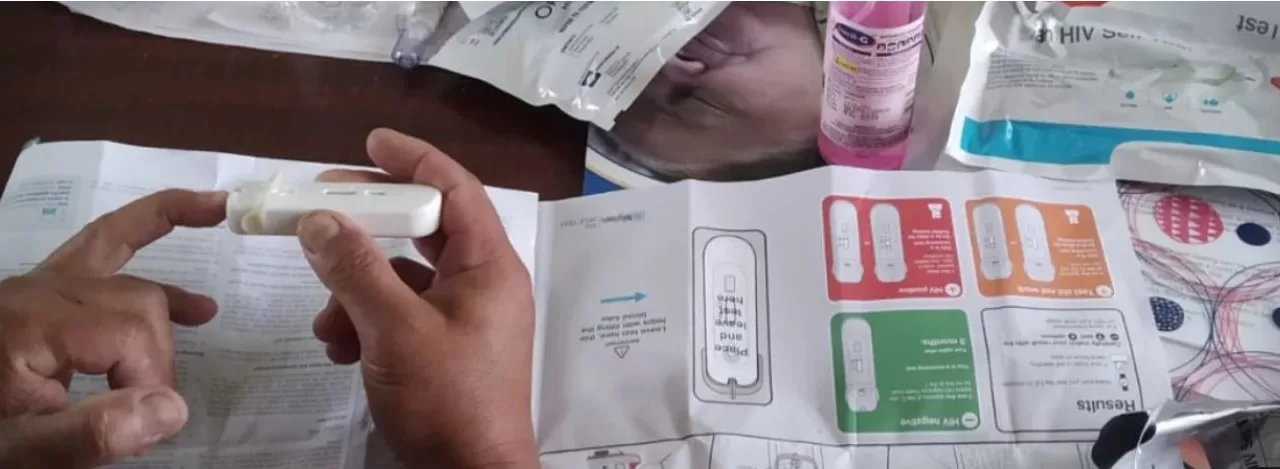
The study, which enrolled 447 participants in five major U.S. cities (Houston, Los Angeles, New York, Philadelphia, and Washington, D.C.), compared two approaches: an intervention arm that provided integrated services, including medication for opioid use disorder (MOUD), antiretroviral therapy (ART) for HIV, and peer navigation, within a mobile health unit, and an active control arm that offered peer navigation to existing community-based services.
The primary findings indicated that at 26 weeks post-randomization, similar proportions of participants in both arms were engaged in MOUD and ART. Specifically, approximately 7% of participants in both groups were alive and on MOUD, about 35% of participants living with HIV had achieved viral suppression, and between 3% and 5% were on HIV pre-exposure prophylaxis (PrEP).
Despite the similar outcome numbers, researchers highlighted the study’s significant retention rate of 90%, particularly among participants with unstable housing. “HPTN 094 provided foundational evidence that mobile units and peer navigation are acceptable in confronting structural and systemic barriers that hinder access to care for addiction and HIV, as well as prevention of HIV,” stated Dr. Steven Shoptaw, HPTN 094 protocol co-chair and professor at UCLA.
Dr. Wafaa El-Sadr, HPTN co-principal investigator, emphasized the importance of meeting individuals where they are, stating, “HPTN 094 met people living with opioid use disorder where they are by designing an intervention that brought integrated and judgment-free health, supported by peer navigation.”
Notably, the study also revealed a trend towards lower mortality in the mobile unit intervention arm, with 70% lower odds of all-cause mortality compared to the control arm, although this was not statistically significant. “More research is needed to confirm the study results and examine the long-term effects of mobile health care units, including their cost-effectiveness and ability to improve health outcomes,” said Dr. Myron Cohen, HPTN co-principal investigator.
The HPTN 094 study is the first randomized controlled trial to evaluate the efficacy of mobile integrated health services for opioid use disorder and HIV prevention or treatment among people who inject drugs in the U.S.
Disclaimer: This news article is based on information provided by the HIV Prevention Trials Network (HPTN) and presented at the 2025 Conference on Retroviruses and Opportunistic Infections (CROI). The information provided is for general knowledge and informational purposes only, and does not constitute medical advice. Readers should consult with a qualified healthcare professional for any health concerns or before making any decisions related to their health or treatment. The findings discussed in this article may require further research and validation. The reported mortality rate differences were not statistically significant, and further research is needed to confirm if mobile health units reduce mortality.