A new study led by researchers from the UMass Chan Medical School Program in Digital Medicine has demonstrated the feasibility and effectiveness of a digital, community-based intervention for patients with chronic obstructive pulmonary disease (COPD). The findings suggest that mobile care can significantly reduce illness-related distress and lower hospitalization rates among COPD patients.
The results from the Healthy at Home study have been published in Pilot and Feasibility Studies and BMC Digital Health. Additionally, a third study evaluating the program’s impact on hospitalization rates is currently under review for publication. A preprint study published on medRxiv reports that patients enrolled in Healthy at Home had a 61% lower chance of readmission within 30 days of hospitalization compared to those who did not participate in the program. The study also indicated a trend toward fewer emergency department visits and shorter hospital stays.
COPD is one of the leading causes of chronic disease-related death in the United States and ranks as the fifth most costly chronic disease, according to the Centers for Disease Control and Prevention (CDC). The Healthy at Home program aimed to address these challenges by integrating digital health solutions into patient care.
Dr. Apurv Soni, principal investigator and co-director of the Program in Digital Medicine, highlighted the unexpected impact of the program. “Even in our relatively small study, the fact that we found statistically significant findings of clinically relevant improvement associated with the use of this technology was really an ‘Aha!’ moment for us,” he said.
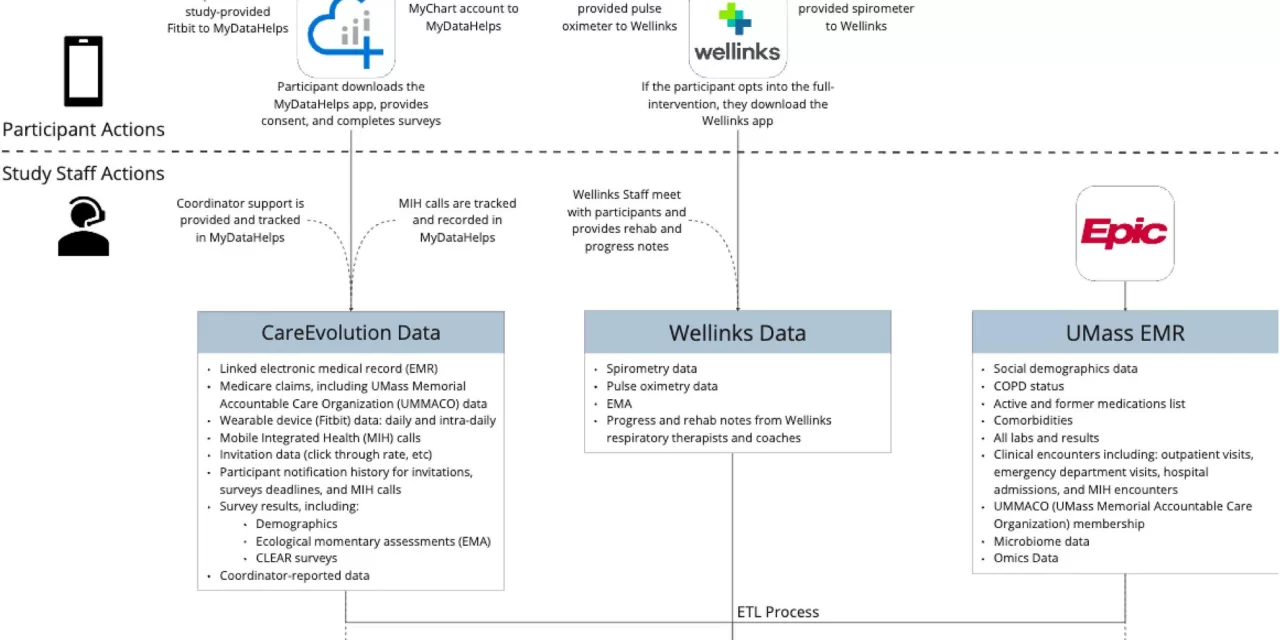
The study was conducted in collaboration with Wellinks, a virtual healthcare company, and CareEvolution, a health data platform. Over an 18-month period, 100 COPD patients at risk of requiring acute care were enrolled in the pilot study. Notably, 96% of participants remained engaged throughout the six-month evaluation period.
The intervention included several key components: home-based mobile integrated health services, a physician-supervised team of paramedics providing 24/7 in-home care, and a digital health dashboard displaying biometric data from wearable sensors. Additionally, Wellinks’ virtual-first COPD management solution offered virtual pulmonary rehabilitation, personalized health coaching, and monitoring via connected devices to measure spirometry and pulse oximetry.
Dr. Soni emphasized the significance of integrating digital medicine with existing clinical systems. “One of the big pushes in digital medicine research, but also in clinical research overall, is how we can integrate clinical trials with the practice of medicine,” he said.
The promising early results have led to the adoption of the Healthy at Home program as a standard of care at UMass Memorial Health through its Digital Health Clinic. Dr. Laurel Caren O’Connor, co-principal investigator, noted that this is one of the first clinical trials to integrate digital tools—such as wearable devices and study apps—with home-based clinical services, enabling comprehensive remote patient monitoring and treatment.
With only 1,700 pulmonary rehabilitation centers available for an estimated 14 million eligible COPD patients in the U.S., researchers believe technology-driven home-based rehabilitation could offer a scalable and effective solution. “If we line up everyone who is eligible for pulmonary rehab, it would take 100 years for them to get treatment,” Dr. Soni pointed out. “The idea of doing this through technology and home-based rehab is something we’re very excited about.”
Looking ahead, the research team has been invited to apply for a major grant from the Patient Centered Outcomes Research Institute to conduct a nationwide clinical trial comparing traditional in-person pulmonary rehabilitation to telepulmonary rehabilitation. Insights from the Healthy at Home trial will play a crucial role in shaping this upcoming study.
Disclaimer: This article is based on findings from published and preprint research studies. While the results are promising, further research and peer-reviewed studies are necessary to validate long-term outcomes. Patients should consult their healthcare providers before making any medical decisions based on digital health interventions.