University of Pittsburgh researchers develop a cutting-edge application that turns smartphones into blood pressure monitors, potentially transforming global hypertension management.
Researchers at the University of Pittsburgh are making waves in the world of blood pressure monitoring with a groundbreaking smartphone application designed to measure pulse pressure using the technology already embedded in our everyday devices. Led by Ramakrishna Mukkamala, a professor of bioengineering at Pitt’s Swanson School of Engineering, this innovation aims to make blood pressure monitoring more accessible, especially for underserved populations.
Mukkamala’s vision was to leverage the widespread use of smartphones to tackle a significant health challenge. “The most significant thing you can do to reduce your risk of cardiovascular disease is to lower high blood pressure through lifestyle changes, but in underserved populations, many people don’t have access to blood pressure cuffs, regular doctor’s appointments, or even know it’s a problem,” Mukkamala explained. “But they do have smartphones.”
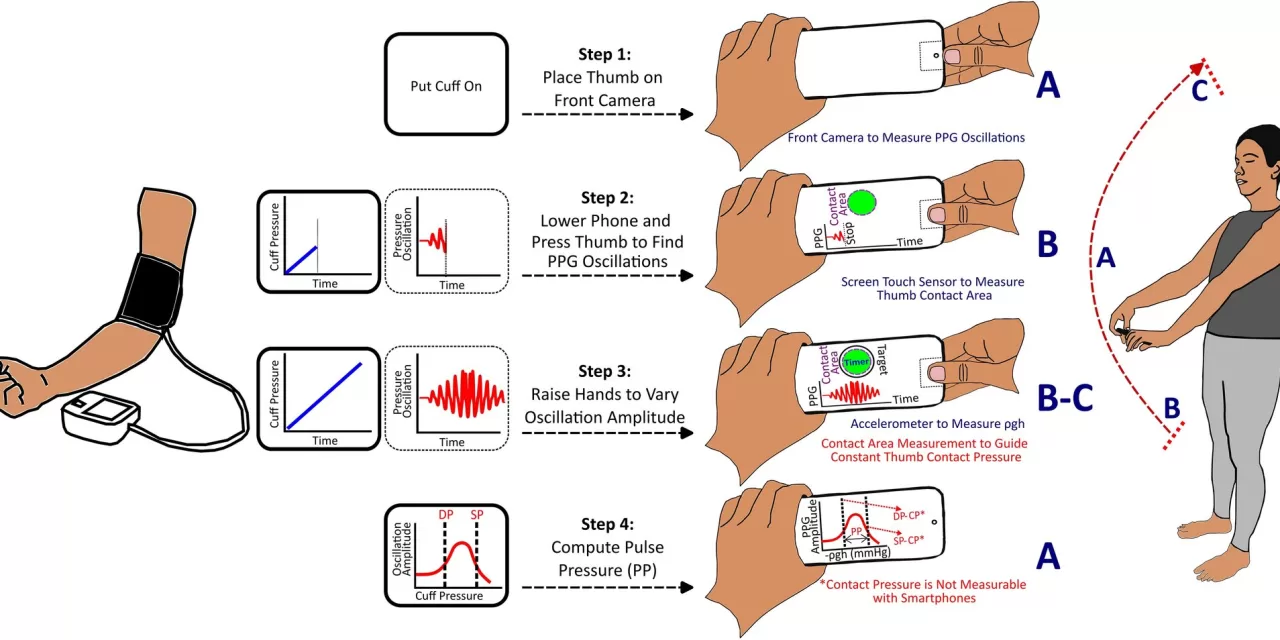
The research team’s solution involves using smartphones’ built-in motion-sensing accelerometers, front cameras, and touch sensors to measure pulse pressure. Users are required to perform a simple hand-raising motion while holding their smartphone to facilitate the measurement. The study, titled “A smartphone application toward detection of systolic hypertension in underserved populations,” published in Scientific Reports, demonstrates a promising technology that could help reduce the global burden of systolic hypertension, particularly in areas with limited access to traditional medical tools.
One of the major challenges was adapting smartphone technology to replicate the effects of a traditional blood pressure exam. Vishaal Dhamotharan, a graduate student involved in the project, noted the difficulty in overcoming the absence of force-sensing tools in smartphones. The team ingeniously utilized gravity to address this challenge. “Because of gravity, there’s a hydrostatic pressure change in your thumb when you raise your hands up above your heart. Using the phone’s accelerometer, we’re able to convert that into the relative change in pressure,” Dhamotharan said.
This method involves guided thumb maneuvers combined with the hand-raising motion to calculate pulse pressure—the difference between the systolic and diastolic blood pressure readings. Although pulse pressure is not commonly used for cardiovascular disease monitoring, the study underscores its potential as an effective metric for detecting hypertension.
Sanjeev Shroff, collaborator and chair of the bioengineering department, sees this development as a significant advancement. “The development of a cuffless blood pressure measurement device that doesn’t require external calibration is the holy grail—such a device currently does not exist. The research work reported in this publication is an important step in the right direction and is encouraging for additional work aimed at obtaining systolic, diastolic, and mean pressures,” Shroff commented.
Hypertension, or high blood pressure, affects over 4 billion adults globally and is a leading modifiable risk factor for cardiovascular disease. This app offers a potential game-changer for managing hypertension by enabling consistent self-monitoring and easy result sharing with healthcare providers. The technology is particularly promising for individuals in low-income settings where access to traditional blood pressure tools is limited.
“This app would be really useful in low-income settings where people may not even have existing access to blood pressure tools,” Dhamotharan said. “Being able to measure blood pressure more frequently would allow an individual to track significant changes, monitor for hypertension, and manage their conditions more effectively.”
As the technology continues to evolve, Mukkamala’s team is committed to improving the app and making it widely available. “The research is here—we just need some help making the technology better,” said Céderick Landry, an assistant professor at the University of Sherbrooke and former postdoctoral researcher in the lab. “This is the first method of its kind, and even better, it’s something that we can start implementing right now.”
With rural communities in the U.S. at higher risk for heart disease compared to urban residents, and similar challenges faced worldwide, this innovation holds the potential to democratize access to crucial health monitoring tools.
For more details, refer to the study published in Scientific Reports: Cederick Landry et al, “A smartphone application toward detection of systolic hypertension in underserved populations,” DOI: 10.1038/s41598-024-65269-w.