Researchers from the Medical College of Georgia (MCG) have made significant strides in understanding why certain treatments for neovascular age-related macular degeneration (AMD) fail to benefit all patients. Moreover, they have developed a promising potential antibody treatment, marking a pivotal moment in combating a leading cause of blindness.
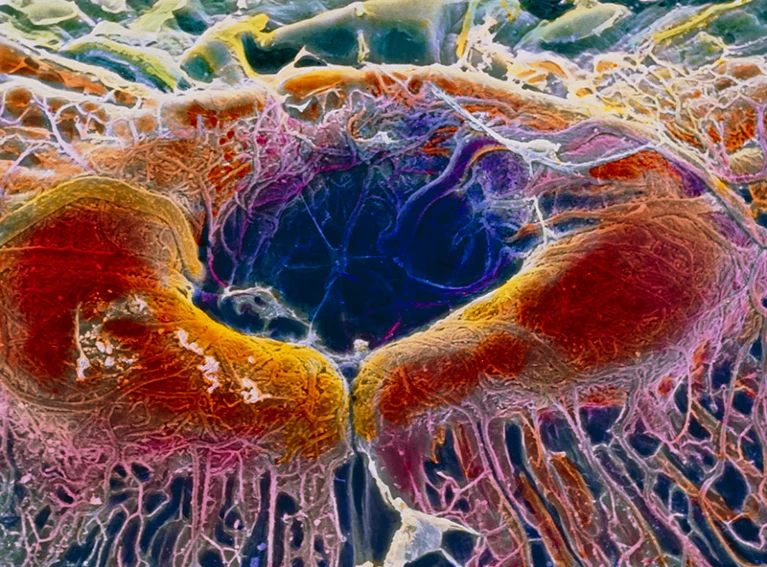
Neovascular AMD is characterized by abnormal blood vessel growth in the back of the eye, specifically the macula, responsible for translating light into image signals. The condition is exacerbated by factors such as older age, diabetes, and obesity, which contribute to excessive vascular growth and macular damage.
Conventionally, Anti-VEGF therapy has been the primary line of defense. This therapy works by blocking vascular endothelial growth factor (VEGF), which curbs excessive blood vessel growth. However, according to the team at MCG, this treatment proves effective for only approximately one-third of patients.
The crux of the issue, the researchers discovered, lies with “fibroblast cells.”
These cells, responsible for producing collagen and various other proteins, accumulate outside vascular cells, leading to fibrosis or scarring in the eye. Consequently, this impedes the efficacy of anti-VEGF treatments by preventing the suppression of excess vasculature.
In a breakthrough study published in the journal Science Translational Medicine, the team elucidated that many fibroblast cells are actually produced by these excessive endothelial cells.
Director of the Vascular Inflammation Programme at MCG’s Vascular Biology Center, Yuqing Huo, highlighted the significance of this finding, stating, “We show, for the first time in this study, that many fibroblast cells are actually produced by these excessive endothelial cells.”
To address this challenge, the researchers targeted the adenosine receptor 2A (Adora2a), a G-protein-coupled receptor found in high levels in the brain, immune cells, and blood vessels. Although crucial in modulating various physiological processes, excessive adenosine can lead to abnormal blood vessel growth.
Using genetically engineered mice prone to developing fibrosis in their eyes, the researchers administered an Adora2a agonist (KW6002) to block the receptor’s function. The results were promising, with the mice demonstrating reduced fibrosis in the eye.
Huo emphasized the potential of this approach, stating, “An antibody could really block both excessive blood vessel growth, the early stage of AMD, and fibrosis, the late stage of AMD. Our findings indicate that blocking Adora2a can certainly target multiple stages of this disease, which might be much more efficient than current treatments.”
This groundbreaking research not only sheds light on the underlying mechanisms of AMD but also paves the way for more effective and targeted treatments, offering hope to millions affected by this debilitating condition.