City of Hope Researchers Unveil a Breakthrough in Thymic Regeneration, With Potential Applications for Cancer Patients and the Aging Population
February 3, 2025 – A team of international scientists led by researchers at City of Hope have made a groundbreaking discovery about the thymus, an essential organ in the immune system. Published today in the journal Immunity, the study outlines a novel mechanism that could enhance thymic function and promote self-repair, offering new hope for individuals whose thymus has been damaged due to aging, stress, or cancer therapies.
The thymus, a small gland located between the lungs and in front of the heart, plays a crucial role in producing T cells, which are vital to the immune system’s ability to fight off pathogens, viruses, and even cancer. However, the thymus is highly susceptible to injury from various factors, including cancer treatments, aging, and stress. When the thymus is compromised, it can lead to a reduced output of T cells, leaving individuals vulnerable to infections and other diseases.
Dr. Andri Lemarquis, the study’s lead author, described the breakthrough: “Our discovery—the recirculation of regulatory T cells back to the thymus—promotes repair through a process that has not been described before and represents a novel pathway to regeneration in the gland. This opens up new possibilities for addressing thymic fatigue and damage.”
A Critical Component of Immunity
Over a lifetime, the body faces countless threats from harmful agents such as bacteria, viruses, and cancer. T cells, generated by the thymus, are the primary defenders against these threats. These immune cells are trained to recognize and neutralize harmful invaders, while also preventing autoimmune diseases by ensuring immune tolerance.
Unfortunately, factors like cancer therapies, aging, and stress can cause the thymus to shrink and lose its ability to produce sufficient T cells, putting patients at greater risk of infections and other complications.
Dr. Lemarquis explained, “Without the ability to regenerate, patients won’t experience immune reconstitution, which is necessary for the production of new protective T cells. Our research aims to find ways to help patients regain this essential immunity.”
Discovering the Key to Thymus Regeneration
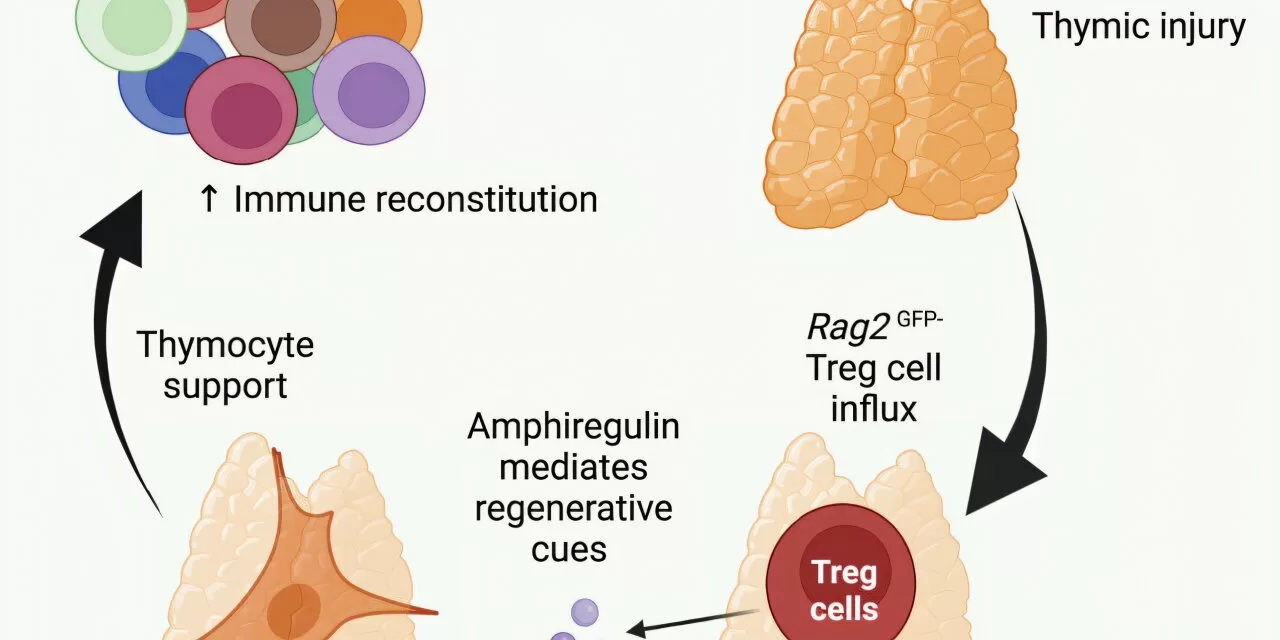
The research team focused on understanding how the thymus responds to injury in two major scenarios: cancer treatments and aging. They studied murine models to observe how the thymus is damaged and how it can begin to recover. Through a combination of advanced imaging techniques and machine learning, the researchers identified a previously unknown population of thymic regulatory T cells (Tregs) that accumulate in the thymus after injury.
These Tregs secrete a growth factor called amphiregulin, which has been shown to stimulate the thymus to regenerate and produce new T cells. Remarkably, the team discovered that when these Tregs were introduced intravenously, they migrated back to the thymus and facilitated its regeneration.
Dr. Lemarquis and his collaborators also tested their findings in human tissue samples, and the results were consistent with those observed in mice, suggesting that this mechanism could be translated to human therapies.
“We were able to confirm that the same pathways operate in both mice and humans,” said Dr. Lemarquis. “This opens up the possibility of using this specific subset of Tregs to regenerate tissues, specifically in the thymus and immune system.”
Implications for Aging and Cancer Patients
One of the most surprising findings of the study was the discovery that even aging thymuses, which were previously thought to be beyond repair, could be rejuvenated using this method. Dr. Lemarquis noted, “If thymic function is lost with age, it can lead to increased mortality due to higher rates of cancers, infections, and autoimmune diseases. Our study shows that even in older mice receiving cancer treatments, we could boost thymic function and enhance immune protection.”
This discovery could have significant implications for aging cancer patients, who are at higher risk of infection and immune deficiencies due to the shrinking of their thymus over time.
Next Steps and Future Applications
The research team plans to expand their studies by analyzing human thymic samples from cancer patients of varying ages to better understand which pathways could be targeted to improve thymic function. They are also exploring the possibility of using synthetic biology to modify T cells to overproduce amphiregulin or other beneficial factors that could accelerate thymic regeneration.
“The potential for Tregs and amphiregulin to be used therapeutically in patients undergoing cancer therapies is immense,” Dr. Lemarquis said. “With the support of our collaborators, we are working to move these findings forward and improve immune function for vulnerable patient populations.”
The study, Recirculating Regulatory T Cells Mediate Thymic Regeneration through Amphiregulin Following Damage, was co-authored by researchers from Memorial Sloan Kettering Cancer Center, the University of Gothenburg in Sweden, Bambino Gesù Children’s Hospital in Rome, New York-Presbyterian Morgan Stanley Children’s Hospital, the University of Washington, Fred Hutchinson Cancer Center in Seattle, and Weill Cornell Medical College in New York.
Disclaimer: This article is based on preclinical research, and the findings have not yet been tested in large-scale human clinical trials. Further studies are necessary to determine the safety and effectiveness of the proposed treatments before they can be applied in clinical settings.
For more information, visit Immunity (DOI: 10.1016/j.immuni.2025.01.006).