Beata Halassy, a virologist from the University of Zagreb, has made headlines by treating her own breast cancer using lab-grown viruses in a self-administered oncolytic virotherapy (OVT) experiment. Halassy’s case raises significant questions about the ethics of self-experimentation in medicine, particularly when it involves emerging therapies and unproven treatments.
Diagnosed with stage 3 breast cancer in 2020 at the site of a previous mastectomy, Halassy, 49, faced the daunting prospect of another round of chemotherapy. After two prior cancer recurrences and an unwillingness to undergo further conventional treatments, she turned to a method that was still largely untested on early-stage breast cancer: OVT.
OVT is a cutting-edge cancer treatment that uses viruses to target and destroy cancer cells while stimulating the immune system to attack the tumor. Halassy, though not a specialist in OVT, had extensive experience with viral research and virus cultivation, giving her the confidence to pursue this experimental route.
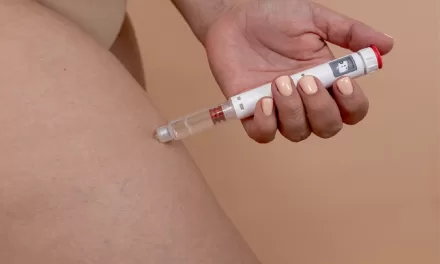
Halassy chose to inject her tumor with two viruses: a strain of the measles virus followed by the vesicular stomatitis virus (VSV). Both viruses had been used in clinical trials for cancer treatment and were known to infect the type of cells her tumor originated from. Over a period of two months, Halassy, with the assistance of a colleague, injected research-grade material directly into the tumor. Her oncologists monitored her progress, prepared to switch to chemotherapy if needed.
The results were promising. Halassy’s tumor shrank significantly, softened, and detached from surrounding tissue, ultimately making it easier to surgically remove. Post-surgery analysis revealed a robust immune response, with the tumor heavily infiltrated by immune cells called lymphocytes, suggesting that the treatment had successfully provoked her immune system to attack both the viruses and the cancer.
Despite the success of her self-treatment, Halassy faced significant ethical scrutiny. Her case report, co-authored with colleagues, was rejected by over a dozen medical journals due to concerns over the ethics of self-experimentation. The major concern, according to Halassy, was the potential for her findings to encourage others to pursue similar unproven treatments. However, Halassy was determined to share her experience, believing that her results could contribute valuable insight into the future of OVT.
Jacob Sherkow, a law and medicine expert at the University of Illinois, acknowledges the ethical complexity of Halassy’s decision. He stresses that while self-experimentation can lead to valuable scientific insights, it also carries risks, particularly in the case of cancer, where patients might be more inclined to try unproven treatments. Sherkow believes the report itself was ethically permissible but argues that it would have been beneficial for a commentary on the ethics of self-experimentation to accompany the case report.
While Halassy’s success may not break entirely new ground in OVT research—since studies are already investigating the use of viral treatments for earlier-stage cancers—her personal experience highlights both the potential and the risks of this emerging therapy. Despite her bold decision to treat herself, Halassy doesn’t believe many people would follow her lead, citing the complexity and expertise required to conduct such a treatment.
Now cancer-free for four years, Halassy’s experience has inspired a shift in her own research focus. She is now investigating the use of OVT to treat cancer in domestic animals, securing funding for this new direction.
Halassy’s story challenges the boundaries of medical ethics and self-experimentation, raising important questions about the intersection of scientific inquiry, personal risk, and the pursuit of innovative therapies.
For more details, refer to the case report published in Vaccines in August.
DOI: https://doi.org/10.1038/d41586-024-03647-0