A breakthrough in non-invasive cardiovascular health monitoring has been achieved by a team of researchers at the University of California, San Diego (UCSD). The team has developed a wearable ultrasound patch that continuously tracks blood pressure in real-time, marking a significant milestone as the first such device to undergo comprehensive clinical validation with over 100 patients.
The findings, published on November 20 in Nature Biomedical Engineering, hold promise for improving blood pressure management both in clinical settings and at home. Unlike traditional blood pressure cuffs that provide only a one-time reading, this patch offers continuous data, capturing fluctuations and trends that can help detect critical patterns.
“Traditional cuff measurements can miss significant changes in blood pressure. Our wearable patch continuously collects blood pressure waveform data, allowing for more accurate trend analysis,” said Sai Zhou, co-first author of the study and recent Ph.D. graduate from UCSD’s Jacobs School of Engineering.
Innovative Design and Technology
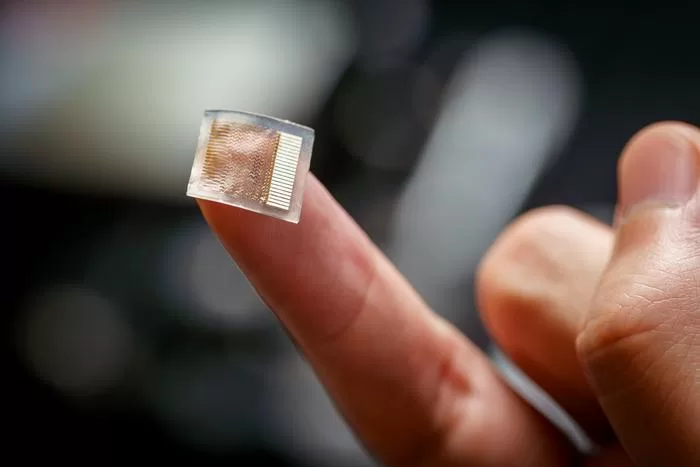
The wearable patch, about the size of a postage stamp, is designed to adhere comfortably to the skin on the forearm. It’s constructed from a silicone elastomer and contains piezoelectric transducers that transmit and receive ultrasound waves. These waves track minute changes in blood vessel diameter, which are then converted into blood pressure readings. The patch is non-invasive, offering precise and continuous blood pressure measurements from deep within the body.
Technological advancements have improved the patch’s performance since its initial prototype. The transducers are now packed more closely together to allow for better targeting of smaller arteries, such as the brachial and radial arteries, which are crucial for accurate readings. A backing layer has also been added to minimize redundant vibrations, enhancing signal clarity and tracking accuracy.
Clinical Validation and Results
The patch has undergone rigorous testing to ensure its accuracy and safety. Over 100 participants took part in studies that simulated real-world conditions, including physical activities, posture changes, and various clinical environments. In tests, the device delivered results comparable to the traditional blood pressure cuff and even to the invasive arterial line, the gold standard for blood pressure monitoring in critical care settings.
In one set of tests, participants wore the patch during daily activities like cycling, mental exercises, and even eating. The patch’s measurements closely matched those of a standard cuff. The device also performed well in clinical tests, where it was worn by patients in cardiac catheterization laboratories and intensive care units. It produced readings that aligned with those of arterial lines, demonstrating its potential as a reliable, non-invasive alternative for continuous blood pressure monitoring.
“We took great care to validate this technology under diverse conditions, from routine activities to intensive clinical settings,” said Sheng Xu, a professor in the Department of Chemical and Nano Engineering at UCSD. “Blood pressure varies greatly due to factors like stress, activity levels, and medications. Testing this device in such varied environments was crucial to ensuring its accuracy and reliability.”
Next Steps and Future Potential
The research team is now preparing for large-scale clinical trials and exploring ways to integrate machine learning to enhance the device’s capabilities. A wireless, battery-powered version is also in development for long-term use, and efforts are underway to ensure seamless integration with hospital systems, offering a potential upgrade to existing cardiovascular monitoring technologies.
This innovative wearable ultrasound patch could transform how blood pressure is monitored, providing more detailed, continuous, and real-time insights into cardiovascular health. As the device moves toward large-scale trials, it could pave the way for broader applications in both clinical care and home monitoring.
This research was supported by a Wellcome Trust Innovator Award and the National Institutes of Health, with all bio-experiments conducted in accordance with ethical guidelines.