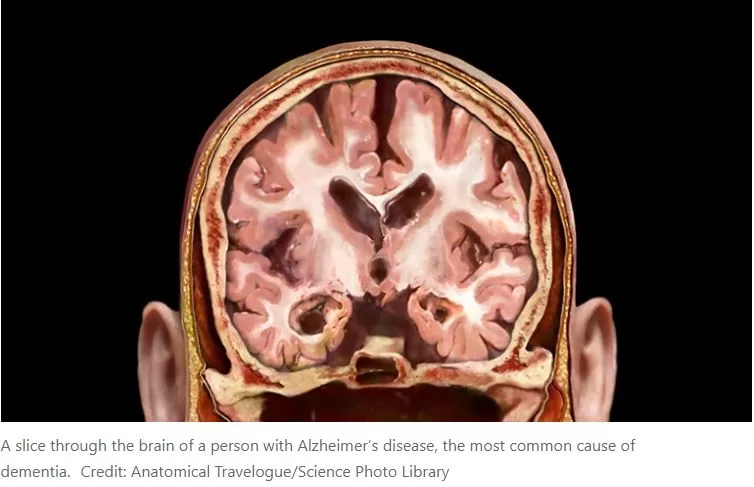
Currently, up to 5.8 million Americans are affected by Alzheimer’s disease, a progressive neurological condition characterized by a decline in cognitive function, including memory loss. The brains of individuals with Alzheimer’s contain protein clumps, primarily beta-amyloid plaques, which are considered a key factor in the development of the disease. Researchers at St. Jude Children’s Research Hospital have identified the crucial proteins involved in the formation of these plaques, as well as a subset of immune cells that appear to suppress their formation. These significant findings were published in Nature Immunology.
Jordy Saravia, Ph.D., co-first author from St. Jude Department of Immunology, highlighted the growing interest in the role of the immune system in neurodegenerative diseases, stating, “We uncovered an important immune cell communication axis that is protective in an Alzheimer’s disease model.” Microglia, specialized immune cells in the brain, are responsible for clearing beta-amyloid plaques. However, as Alzheimer’s progresses, they may lose this ability, potentially leading to the production of inflammatory substances that contribute to plaque formation. The St. Jude researchers discovered that boosting another type of immune cell, known as CD8+ T cells, is crucial in slowing down this process. This interaction with microglia proves essential in reducing beta-amyloid accumulation and preserving cognitive functions in a mouse model of the disease.
Wei Su, Ph.D., co-first author from St. Jude Department of Immunology, emphasized that their study is the first to demonstrate the protective role of a subpopulation of CD8+ T cells in an Alzheimer’s disease mouse model. Moving forward, this work may pave the way for effective interventions in neurodegenerative diseases.
While previous research has highlighted the intricate roles of T cells and other immune system components in Alzheimer’s disease, the St. Jude scientists showed that CD8+ T cells with suppressive features accumulate in the brains of both mouse models and Alzheimer’s patients. This underscores the complex role of T cells in this disease.
Corresponding author Hongbo Chi, Ph.D., from St. Jude Department of Immunology, emphasized the need for a deeper understanding of these intricate neuro-immune interactions to enhance outcomes for this neurodegenerative disease.
To comprehend how T cells were slowing symptom progression in their Alzheimer’s disease model, the St. Jude team investigated the most prevalent molecular interaction between CD8+ T cells and microglia. They identified a protein on the surface of CD8+ T cells, CXCR6, that interacts with the protein CXCL16 expressed by microglia. This interaction functions as a form of communication between the two cells, similar to a human handshake conveying information.
Chi explained, “We found CD8+ T cells use CXCR6 to interact with CXCL16 from microglia. Moreover, CD8+ T-cell accumulation, localization, and function in the brain are regulated by CXCR6.”
The scientists determined how this interaction delays the onset of Alzheimer’s disease-related pathologies. CD8+ T cells position themselves next to the microglia, which are located adjacent to the beta-amyloid plaques. They then use this “handshake” to signal to the microglia to cease uncontrolled inflammation, subsequently slowing plaque growth and alleviating symptoms in the mouse models.
When the researchers deleted the gene for the CD8+ T cell’s protein CXCR6, the mice exhibited more severe Alzheimer’s disease-related symptoms. This was partly due to the CD8+ T cells lacking CXCR6, failing to accumulate in the brain near the microglia or plaque site, and not acquiring the necessary suppressive function. Thus, disrupting the CD8+ T cell’s ability to perform this “handshake” hindered its protective effect against Alzheimer’s disease symptoms.
Chi summarized their major findings, stating, “One is the crucial role of CD8+ T cells in maintaining brain homeostasis, thereby providing a protective role in Alzheimer’s disease.” Homeostasis involves the process of keeping a system in a relatively stable state, in this case, CD8+ T cells working to limit disruptions caused by microglia dysfunction and Alzheimer’s disease-related plaques. “The other major finding is identifying the central importance of the T cell protein CXCR6 for CD8+ T-cell accumulation and function in the brain,” Chi continued. “We really need to characterize these kinds of neuro-immune interactions better. Only by understanding this basic biology can we advance the field and find new treatments.”