Addressing the specific sleep patterns of adolescent “night owls” is crucial for aligning their biological rhythms with their educational requirements. Many school systems are not designed to accommodate those who naturally sleep and wake up later, potentially contributing to higher rates of depression in this demographic. Researchers at UC San Francisco have developed an intervention to help these teenagers harmonize their sleep cycles with their school commitments, offering hope for those grappling with depression.
While 40% of teenagers in general identify as night owls, this number rises to 80% among those experiencing depression. The key to the success of the intervention lies in guiding these night owls to structure their lives in a way that allows them to sleep in as much as possible, while gradually adjusting their bodies to an earlier sleep schedule. Lauren Asarnow, a clinical psychologist at UCSF Health specializing in sleep health, emphasizes the significance of this discovery, highlighting that for a certain subset of teens, prioritizing sleep is particularly vital for alleviating depression symptoms. Additionally, they must be empowered to lead a lifestyle that aligns more closely with their natural sleep-wake patterns.
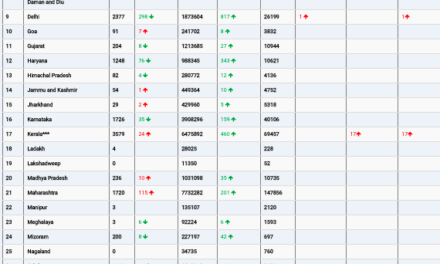
Published in August in the Journal of Child Psychology and Psychiatry, the study analyzed data from 42 participants with clinical depression, a subset of a larger group of 176 night-owl adolescents. Of these, 24 received the Transdiagnostic Sleep and Circadian Intervention (TransS-C), while 18 received educational sessions on leading a healthy lifestyle. Throughout the study, all participants maintained sleep diaries and used devices to monitor the quality of their sleep. They also attended weekly 45-minute therapy sessions for eight weeks.
At the outset, all teens scored at least 40 on the Children’s Depression Rating Scale, indicating clinically significant depression. A score of 28 or lower indicates remission. Six months after the treatment, the intervention group’s average score had dropped to 21.67, compared to 32.5 for the group that received the healthy lifestyle intervention. At the 12-month mark post-treatment, the intervention group scored 24.97, while the control group registered 32.75.
A larger study, funded by the National Institute of Mental Health, is set to enroll 200 teens in the Bay Area in the upcoming fall season. Each year, around 3 million adolescents experience at least one major depressive episode, and approximately 40% do not respond to treatment. Research indicates that teens who naturally tend to fall asleep and wake up later are at a heightened risk of recurrent and more severe depression, suicidality, and poor response to antidepressant treatment. Asarnow underscores the importance of understanding that attributing these traits to laziness is misguided, emphasizing that often it is simply a matter of biology and not the individual’s fault.