As highlighted in a presentation during a Hot Line session at ESC Congress 2023, the use of blood thinners (anticoagulants) leads to bleeding complications without offering stroke prevention benefits for individuals with atrial high rate episodes (AHRE) but without electrocardiogram (ECG)-diagnosed atrial fibrillation. The results of this research were published in the New England Journal of Medicine.
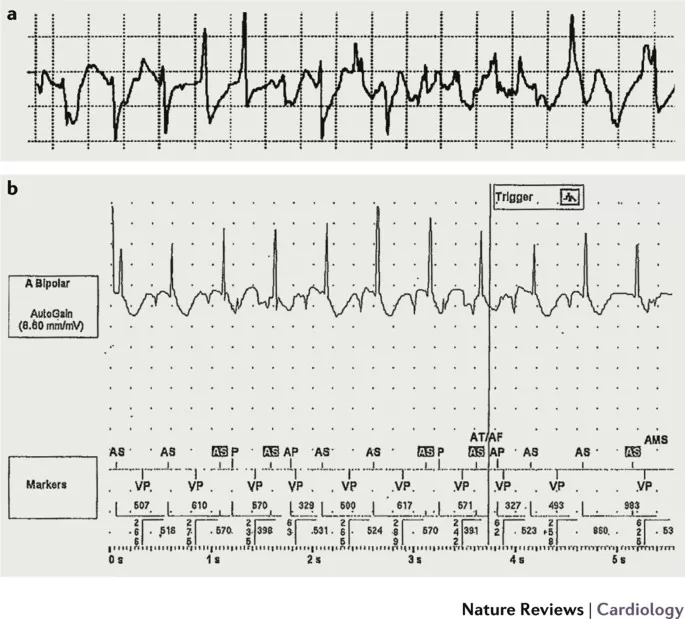
Anticoagulants are effective in preventing strokes among individuals with atrial fibrillation, but their efficacy is limited in those without such conditions, including individuals with heart failure. Atrial high-rate episodes (AHRE) are infrequent and brief atrial arrhythmias resembling atrial fibrillation, detected by implanted devices like pacemakers, defibrillators, and loop recorders. AHRE occurs in 10% to 30% of individuals with implanted devices. Despite a heightened stroke risk in AHRE patients, this risk remains lower than in those with atrial fibrillation.
For individuals with atrial fibrillation and a heightened stroke risk, ESC recommendations endorse oral anticoagulation to mitigate stroke risk. However, for patients with AHRE but lacking ECG evidence of atrial fibrillation, personalized decisions are advised.
The inaugural NOAH-AFNET 6 trial investigated the effectiveness and safety of oral anticoagulation in individuals with atrial high-rate episodes (AHRE) but lacking ECG-confirmed atrial fibrillation. This randomized, double-blind, double-dummy trial pitted the anticoagulant edoxaban against a placebo in patients aged ≥65 years. These patients had AHRE episodes lasting ≥6 minutes, as detected by implanted devices, and possessed at least one additional stroke risk factor (such as heart failure, hypertension, diabetes, previous stroke or transient ischemic attack, vascular disease, or age ≥75 years). It’s worth noting that this patient group was beyond the approved use of edoxaban.
Spanning 206 sites across 18 European countries, participants were randomly assigned in a 1:1 ratio to receive either anticoagulation or no anticoagulation. The anticoagulation arm involved edoxaban at a dose approved for stroke prevention in atrial fibrillation (60 mg once daily, potentially reduced to 30 mg once daily based on approved dose reduction criteria for atrial fibrillation stroke prevention). The no anticoagulation group received either placebo with no active components or aspirin at a daily dose of 100 mg for patients requiring antiplatelet therapy. The primary outcome assessed was a combination of stroke, systemic embolism, or cardiovascular death. Additionally, a safety outcome was measured, which combined major bleeding events and all-cause mortality. All enrolled patients were followed until the study’s conclusion.
The primary analysis of modified intention-to-treat included 2,536 patients who received at least one dose of the study drug. These patients were elderly and presented with multiple stroke risk factors, boasting an average age of 78 years. Of the participants, 37% were women, and the median CHA2DS2-VASc score was 4.5. The baseline median duration of atrial high-rate episodes (AHRE) was 2.8 hours, with no upper limit, and 97% of these episodes displayed atrial rates surpassing 200 beats per minute, bearing a strong resemblance to atrial fibrillation.
The trial was prematurely halted due to safety signals and a tendency towards futility in terms of efficacy following the enrollment of all intended patients. In terms of the primary efficacy outcome, 83 patients in the anticoagulation group (3.2% per year) experienced it, while 101 patients in the no anticoagulation group (4.0% per year) did, resulting in a hazard ratio (HR) of 0.81 (with a 95% confidence interval [CI] of 0.6-1.1; p=0.15). Stroke rates were low in both randomized groups, at 1.1% per year without anticoagulation and 0.9% per year with anticoagulation. As for the primary safety outcome, 149 patients in the anticoagulation group (5.9% per year) encountered it, compared to 114 patients in the no anticoagulation group (4.5% per year), yielding an HR of 1.3 (95% CI 1.0-1.7; p=0.03). This difference in safety outcomes was driven by the anticipated rise in major bleeding incidents among patients on anticoagulation (HR 2.10; 95% CI 1.30-3.38; p=0.002). Among the total participants, 462 out of 2,536 (18%; 8.7% per year) were diagnosed with atrial fibrillation through ECG.
Principal investigator Paulus Kirchhof from the University Heart & Vascular Center in Hamburg, Germany, commented: “The NOAH-AFNET 6 trial demonstrated that administering oral anticoagulation to patients with AHRE increases bleeding occurrences without reducing the combined occurrence of stroke, systemic embolism, or cardiovascular death. The anticipated increase in bleeding incidents with anticoagulation was observed. The unexpectedly low stroke rates with and without anticoagulation warrant attention. The findings from NOAH-AFNET 6 underscore the importance of requiring ECG confirmation of atrial fibrillation before initiating oral anticoagulation. Further research is essential to gain a better understanding of stroke risk in individuals with infrequent and brief atrial arrhythmias.”
Source ANI










