Situation at a Glance
Description of the Situation
On 22 March 2024, the Timor-Leste Ministry of Health and the Ministry of Agriculture, Fishery and Forestry, reported to the World Health Organization (WHO) its first confirmed fatal human case of rabies. The case is a 19-year-old female from Pasabe Sub-Region, Oecusse, formally known as the Special Administrative Region of Oe-Cússe Ambeno (RAEOA – Portuguese acronym). The case was confirmed by Real-Time Polymerase Chain Reaction (RT-PCT) at the National Health Laboratory in Timor-Leste on 22 March from a saliva sample taken prior to the individual’s death.
On 20 March, the patient presented to a local health center with symptoms including high fever, vomiting, sore throat, cough, difficulty swallowing food, hydrophobia, photophobia, back pain, and neck stiffness. It was reported that she was bitten on the hands by a dog on 26 December 2023 in Oecusse. During the investigation, residents described the dog as very aggressive, and reported that it had not bitten anyone else. The dog died and was buried on 27 December 2023. The patient had not received rabies post-exposure prophylaxis (PEP) after the dog bite. On 21 March, she was transferred to Guido Valadares National Hospital (HNGV) in the capital city of Dili and died on 22 March 2024.
During 2024, as of 26 March, a total of 29 suspected rabies cases exposed to dogs in Oecusse Municipality, RAEOA, were reported. All suspected cases have been administered the Tetanus Toxoid (TT) and Rabies PEP vaccines. However, the Rabies Immune Globulin (RIG) serum could not be provided because it was out of stock.
It should be noted that Oecusse is an enclave of Timor-Leste located within Indonesia East Nusa Tenggara province (NTT) where between 1 January and 15 March 2024, six human rabies deaths have been recorded. In 2023, a total of 30 human rabies deaths were reported from NTT province.
Epidemiology
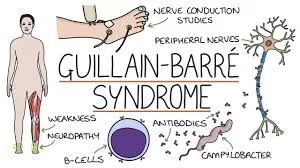
Rabies is a vaccine-preventable, zoonotic, viral disease affecting the central nervous system. Once clinical symptoms appear, rabies is nearly 100% fatal. In up to 99% of cases, domestic dogs are responsible for rabies virus transmission to humans. Yet rabies can affect both domestic and wild animals. It spreads to people and animals via saliva, usually through bites, scratches or direct contact with mucosa (e.g. eyes, mouth or open wounds). Children between the ages of 5 and 14 years are frequent victims. Direct human-to-human transmission has never been documented, however it has occurred from infected organ/tissue donors to transplant recipients.
The incubation period for rabies is typically 2–3 months but may vary from 1 week to 1 year, depending on factors such as the location of virus entry and the viral load. Initial symptoms of rabies include generic signs like fever, pain and unusual or unexplained tingling, pricking, or burning sensations at the wound site. As the virus moves to the central nervous system, progressive and fatal inflammation of the brain and spinal cord develops. Clinical rabies in people can be managed but very rarely cured, and not without severe neurological deficits. Rabies deaths occur mainly in those who cannot immediately access effective post-exposure prophylaxis. According to the Union Against Rabies Forum (launched by FAO, WHO and WOAH), globally, every nine minutes one person dies from rabies. Almost half of them are children.
People can be protected against rabies through a vaccine given to individuals as pre-exposure or post-exposure prophylaxis. Post-exposure prophylaxis is the emergency response to a rabies exposure. This prevents the virus from entering the central nervous system, which would invariably result in death.
Public Health Response
The Timor-Leste Ministry of Health has taken the following public health response actions:
- Dog vaccination has been conducted in the Municipalities of Covalima, Bobonaro, and RAEOA, achieving a coverage rate of 70% as of 25 March 2024. Dog vaccination is ongoing with a target to achieve 100% coverage.
- Risk communication to raise community awareness via social media, community campaign and press conference, advising citizens residing in the border area to vaccinate their dogs, avoid contact with wild animals, observe if there are any changes in dog behavior, report dog bite incidents for immediate treatment and rabies vaccination.
- Providing training to healthcare workers in all health care facilities on investigation and clinical management of suspected rabies exposures.
- Implementing active surveillance, with all dog bite cases now required to be reported to the Community Health Centers (CHCs) with necessary information recorded and provided with appropriate case management.
- Ensuring availability of rabies vaccines and human rabies immunoglobulin (HRIG) in all CHCs and regional referral hospitals.
- Organising Rabies Tripartite Expert Mission to Timor-Leste with Food and Agriculture Organization (FAO), WHO and World Organization for Animal Health (WOAH).
WHO procured 1000 doses of human rabies vaccines and distributed them to hospitals and health clinics. Collaboration between the Timor-Leste Ministry of Health and WHO is ongoing to provide additional anti-rabies vaccines and RIG to individuals who have been exposed to a suspected rabid animal.
WHO Risk Assessment
The risk at the national level is assessed as ‘High’ due to the following:
- The country was previously classified as “rabies free” and has now reported the first confirmed human case. As such, experience and awareness of community and health care workers on rabies are likely limited.
- Oecusse, the municipality where the current case was bitten and reported from, is an enclave of Timor-Leste located within East Nusa Tenggara province (NTT) in Indonesia where rabies is endemic in both dogs and humans.
- Current dog vaccination coverage in NTT province, Indonesia is only 5.5% and dog vaccine coverage in Indonesia in 2022, was 24%, while 70% coverage is needed as the main technical control measure.
- Timor-Leste has a significant population of stray and unvaccinated dogs including in the areas bordering Indonesia.
- Insufficient stock of human rabies vaccines in the government health facilities.
- The health workers have limited knowledge about rabies case management, dog bite and scratch case management.
- Inadequate veterinary services, including the lack of regular canine vaccination campaigns against rabies, a lack of stock of canine rabies vaccines and inadequate laboratory capacity for rabies testing
- Not all humans bitten by a suspected rabid animal (mainly dogs) receive adequate and timely PEP, due to several reasons including lack of awareness among the general population and health workers, and lack of vaccination and RIG.
- NTT province in Indonesia shares land borders with Timor-Leste, and control measures to limit the movement of animals, particularly unvaccinated dogs, across these borders is challenging due to the terrain and extent of the land border.
Since Timor-Leste’s only land border is with NTT province in Indonesia, which is already endemic for rabies (humans and canines), the risk of the international spread of rabies from Timor-Leste to other countries is unlikely. Available data indicates only the current one fatal case of rabies in Timor-Leste, with no links to international travel, tourism or international gatherings.
WHO Advice
Although highly effective animal vaccines have been available for over a century, rabies remains present on all continents except Antarctica. Rabies is included in WHO’s 2021–2030 Roadmap for the Global Control of Neglected Tropical Diseases, which sets regional, progressive targets for the elimination of targeted diseases. Rabies elimination is feasible and achievable if this goal is prioritized and financially and politically supported. The key to implementing effective rabies elimination programs is to engage with local communities, start small, catalyze long-term investment through stimulus packages, ensure the ownership of governments, demonstrate success and cost-effectiveness, and scale up quickly.
As a zoonotic disease, rabies requires close cross-sectoral coordination at the national, regional and global levels, including:
- Risk Communication and Community Engagement (RCCE): Raising awareness of rabies disease through engaging communities and empowering people to seek early treatment whenever they are exposed to a rabid animal. This includes an understanding of how to prevent rabies in animals, when to suspect rabies, and what to do in case of exposure.
- Immunization of persons: Very effective rabies vaccines and rabies immunoglobulins are available to immunize people after suspected exposure to rabies (post-exposure prophylaxis). Appropriate wound management and prompt access to quality-assured PEP are almost 100% effective in preventing human rabies deaths. Pre-exposure prophylaxis (PrEP) is recommended for people in certain high-risk occupations (such as laboratory workers handling live rabies and rabies-related viruses) and people whose professional or personal activities might lead to direct contact with bats or other mammals that may be infected with rabies (such as animal disease control staff and wildlife rangers). PrEP might also be indicated for outdoor travellers and people living in remote, highly rabies-endemic areas with limited local access to rabies biologics.
- Mass dog vaccination: As dogs transmit up to 99% of human rabies cases, the control and elimination of rabies in dogs prevents rabies at its source. Vaccinating dogs, including puppies, is the most cost-effective strategy for preventing rabies in people, and reduces the need for PEP. Mass dog vaccination with high quality and safe vaccines, aiming at 70% coverage in endemic areas interrupts Rabies virus (RABV) transmission at its animal source and saves human lives. Education on dog behaviour and bite prevention for both children and adults is an essential extension of rabies vaccination programs and can decrease both the incidence of human rabies and the financial burden of treating dog bites.
- Wildlife vaccination: Oral rabies vaccination for use in wildlife is available with efficacy claims for several wildlife species, such as foxes, raccoon dogs, wolves, coyotes and raccoons.
This event does not interfere with travel and trade. Travellers must be made aware of the risk of contracting rabies while traveling to rabies-endemic countries.
Further Information
- WHO Rabies fact sheet
- Rabies Vaccine: WHO position paper- April 2018
- WHO. Zero by 30: The global strategic plan to end human deaths from dog-mediated rabies by 2030
- WOAH, Rabies
- WHO. Strategic framework for elimination of human rabies transmitted by dogs in the South East Asia Region
- United Against Rabies, FAO, WHO and WOAH forum
- Rupprecht CE, Fooks AR, Abela-Ridder B, editors. Laboratory techniques in rabies, fifth edition. Volume 2. Geneva: World Health Organization; 2018. Licence: CC BY-NC-SA 3.0 IGO
Citable reference: World Health Organization (10 April 2024). Disease Outbreak News; Rabies – Timor-Leste. Available at: https://www.who.int/emergencies/disease-outbreak-news/item/2024-DON513