A good night’s sleep sets the foundation for a productive day. However, for nearly a quarter of American adults struggling with mental illness, restful sleep remains elusive.
For individuals battling psychiatric conditions such as addiction or mood disorders like depression, disrupted sleep can worsen symptoms and hinder treatment effectiveness. Despite the significant role that circadian rhythms and sleep play in addiction, neuroscientists are only now beginning to unravel the molecular mechanisms behind this connection.
The Link Between Sleep and Addiction
Addictive substances and sleep disturbances have a deeply intertwined relationship. Many addictive drugs alter sleep-wake cycles, and people with substance use disorders frequently experience disrupted sleep. These sleep disturbances are linked to increased addiction severity and higher relapse rates. While this presents a “chicken-or-egg” dilemma, it also provides an opportunity for researchers to explore how the sleep-addiction connection might inform new treatment strategies.
Circadian Rhythms and Health
At the core of the relationship between sleep and mental health are circadian rhythms, the body’s internal clock. These biological rhythms synchronize bodily functions with environmental cues, ensuring that various physiological processes, such as hormone release and metabolism, align with the day-night cycle.
Circadian disruptions, such as those caused by frequent night shifts or irregular sleep schedules, have been linked to serious health issues, including cardiovascular disease and diabetes. For individuals with addiction, these disruptions can be even more pronounced, leading to increased cognitive impairment and emotional instability.
Opioid Addiction and Sleep Disruptions
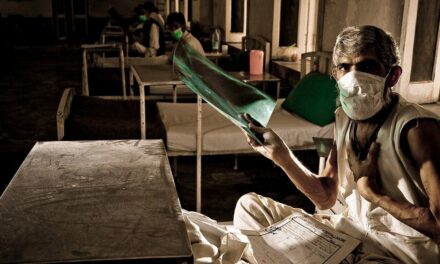
The opioid crisis continues to claim tens of thousands of lives annually in the U.S., with limited treatment options available. People struggling with opioid addiction often exhibit disrupted sleep patterns and imbalances in key stress-regulating hormones. These disturbances can worsen both mental and physical health, increasing the risk of relapse.
Recent studies in both humans and mice have highlighted the significant impact of opioid use on circadian rhythms. Research has revealed that individuals with opioid addiction display altered gene expression patterns in critical brain regions associated with addiction. Some genes lose their natural rhythm, while others adopt an entirely different cycle of activity.
Potential for New Treatments
One promising area of research involves the NPAS2 gene, a key component of the molecular clock. Researchers found that NPAS2 activity is significantly altered in individuals with opioid addiction. Blocking NPAS2 function in mice led to increased fentanyl-seeking behavior, particularly in female mice, suggesting a potential link between circadian regulation and opioid use disorder.
Further studies suggest that restoring circadian balance and improving sleep quality may help reduce opioid cravings and lower relapse rates. These findings highlight the importance of exploring sleep-focused interventions for addiction treatment.
Looking Ahead
The intricate relationship between sleep and addiction underscores the need for further research. Understanding how circadian rhythms influence addiction could lead to innovative treatment approaches targeting molecular pathways such as NPAS2.
Quality sleep isn’t just essential for well-being—it may also serve as a critical tool in combating opioid addiction and reducing overdose rates.
Disclaimer: This article is for informational purposes only and should not be considered medical advice. If you or someone you know is struggling with addiction, seek professional help from a healthcare provider or addiction specialist.