New research highlights the ongoing need for COVID-19 protection for individuals with weakened immune systems, emphasizing how scalable tests can identify those most at risk and guide tailored protection strategies.
Published in The Lancet, the study conducted by experts from the University of Nottingham and Nottingham University Hospitals NHS Trust, introduces a simple blood test that can predict the severity of COVID-19 infection. This breakthrough allows for personalized approaches to vaccination and enhanced protection for vulnerable individuals.
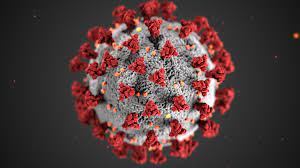
The MELODY Study (Mass Evaluation of Lateral Flow Immunoassays for the Detection of SARS-CoV-2 Antibody in Immunosuppressed People) aimed to evaluate how well immunosuppressed individuals develop antibodies following at least three COVID-19 vaccinations. Antibodies are essential in defending the body against infections, yet immunosuppressed patients may experience a reduced response to vaccines.
With over 28,000 participants, the MELODY Study is the largest study of its kind. Immunosuppressed populations, often overlooked in COVID-19 research, were the focus. The study was led by experts at Imperial College London, with Dr. Fiona Pearce from the University of Nottingham’s School of Medicine serving as the senior joint author.
“By utilizing national disease registration, we have successfully included groups that are typically excluded from research, including over 6,000 individuals with rare autoimmune rheumatic diseases. This breakthrough, facilitated by the RECORDER group and the National Disease Registration Service at NHS England, represents an important step forward,” said Dr. Pearce.
From December 2021 to June 2022, participants used home-testing kits to measure long-lasting antibody levels, using methods from the REACT Study—one of the world’s largest and most comprehensive coronavirus monitoring initiatives. Unlike standard COVID-19 tests, these kits assessed immune protection.
The study found that 82% of immunosuppressed patients developed antibodies after vaccination. Those with detectable antibodies were less likely to contract the virus or require hospitalization if infected.
Dr. Willicombe, Clinical Reader at Imperial College London and Honorary Consultant Nephrologist, emphasized that while most patients responded well to vaccination, certain immunosuppressive treatments may diminish vaccine efficacy. “MELODY has shown that we can individually assess vaccine response and the risk of severe outcomes, supporting personalized approaches to COVID-19 prevention, such as tailored vaccination schedules or treatments,” Dr. Willicombe said.
Dr. Peter Lanyon further stressed the importance of keeping immunosuppressed individuals up to date with all eligible vaccinations, including COVID-19 and flu, to ensure maximum protection.
The study’s findings underscore the need for adaptive health measures to address the needs of vulnerable groups, ensuring equitable access to advancements in medicine and public health.
Disclaimer: The information provided here is based on research published in The Lancet and is intended for informational purposes only. For personal medical advice, please consult a healthcare provider.