A recent study originating from Sweden has sent shockwaves through the medical community, revealing a chilling truth: obesity’s impact on health stretches far beyond what was previously understood. It’s not merely about heart disease or diabetes anymore; obesity is now solidly linked to a staggering 32 different types of cancer, potentially contributing to a massive 40% of all cases.
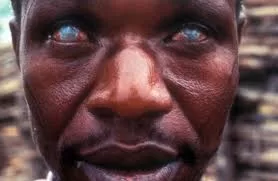
The study, while confirming the existing connection between obesity and some cancers like breast and bowel cancer, unveils a far broader scope of risk. It implicates excess weight in the development of several other cancers not previously associated with obesity, including malignant melanoma and gastric tumors.
Moreover, less common cancers such as those in the small intestine and pituitary gland, alongside head and neck cancers, as well as vulvar and penile cancers, are now also on the list of malignancies potentially fueled by excess weight.
This expanded understanding significantly broadens the scope of obesity’s impact on cancer risk. The findings underscore the urgency of addressing the obesity epidemic not only for its known impacts on cardiovascular health and diabetes but also for its far-reaching implications in cancer prevention and treatment.
Understanding the Biological Mechanisms
Scientists are piecing together the complex puzzle of how obesity wreaks havoc on our bodies. Chronic low-grade inflammation, disrupted insulin signaling, altered hormone levels, and gut microbiome imbalances are key factors contributing to the link between obesity and cancer.
Chronic inflammation, a known risk factor for cancer, can result from excess fat tissue secreting pro-inflammatory cytokines. Disrupted insulin signaling and elevated insulin and IGF-1 levels promote cancer growth, particularly in insulin-responsive tissues. Altered hormone levels, particularly elevated estrogen exposure, have been directly linked to increased risks of certain cancers. Additionally, obesity can alter the gut microbiome, leading to systemic inflammation and potentially increasing cancer risk.
The Urgency of Action
The research demonstrates a clear and alarming link between a person’s Body Mass Index (BMI) and their likelihood of developing cancer. With every five-point increase in BMI, the risk of several common cancers significantly rises, emphasizing the importance of maintaining a healthy weight as a crucial component of cancer prevention.
The implications of this research are staggering. With obesity rates soaring worldwide, urgent action is needed to combat this looming cancer tsunami. Strategies such as promoting healthy eating, physical activity, and access to affordable, nutritious food are now more critical than ever.
Economic Ramifications
Obesity-related cancers place a substantial strain on healthcare systems due to their complex and costly nature, leading to higher medical expenses. Moreover, reduced productivity in the workforce due to obesity-related health problems exacerbates economic losses, underscoring the need for comprehensive public health initiatives to address obesity and its associated health risks.
Making Informed Choices
While the study’s findings are grim, they offer a glimmer of hope. By understanding the link between obesity and cancer, individuals can make informed choices to improve their health. Even small changes in lifestyle, such as incorporating more fruits and vegetables into diets and increasing physical activity, can have a profound impact on well-being.
In conclusion, this research serves as a clarion call for action. Prioritizing obesity prevention and treatment is crucial not only for improving individual health outcomes but also for safeguarding economic stability and prosperity. By working together, we can create a healthier future where the shadow of obesity no longer looms large over our lives.