January 17, 2025 | Source: Frontiers of Medicine
Nipah virus (NiV), a zoonotic paramyxovirus, continues to pose a significant global health threat, attracting attention for its high fatality rates and potential for human-to-human transmission. First identified in Malaysia in 1998, NiV has since caused multiple outbreaks, particularly across South and Southeast Asia, with alarming consequences for public health. A recent review titled “Nipah virus: epidemiology, pathogenesis, treatment, and prevention,” published in the journal Frontiers of Medicine, delves into the latest research on the virus, shedding light on its features and the urgent need for enhanced global vigilance.
The Origins and Spread of Nipah Virus
NiV’s primary natural reservoir is the fruit bat, particularly species within the Pteropus genus, which can transmit the virus to humans through contaminated food sources or direct contact with infected animals. Pigs, which can act as intermediate hosts, have played a central role in facilitating human outbreaks. The virus has affected countries such as Malaysia, Singapore, Bangladesh, India, and the Philippines, with numerous human infections reported, underscoring the widespread risk of transmission.
The virus’s ability to infect a variety of hosts, from bats to domestic animals, combined with its potential for human-to-human spread, makes NiV especially concerning. The review highlights two primary genetic lineages of NiV—NiV-MY and NiV-BD—which differ in their pathogenicity and transmissibility, with NiV-MY being more frequently associated with human outbreaks.
The Pathogenesis and Clinical Manifestations of NiV
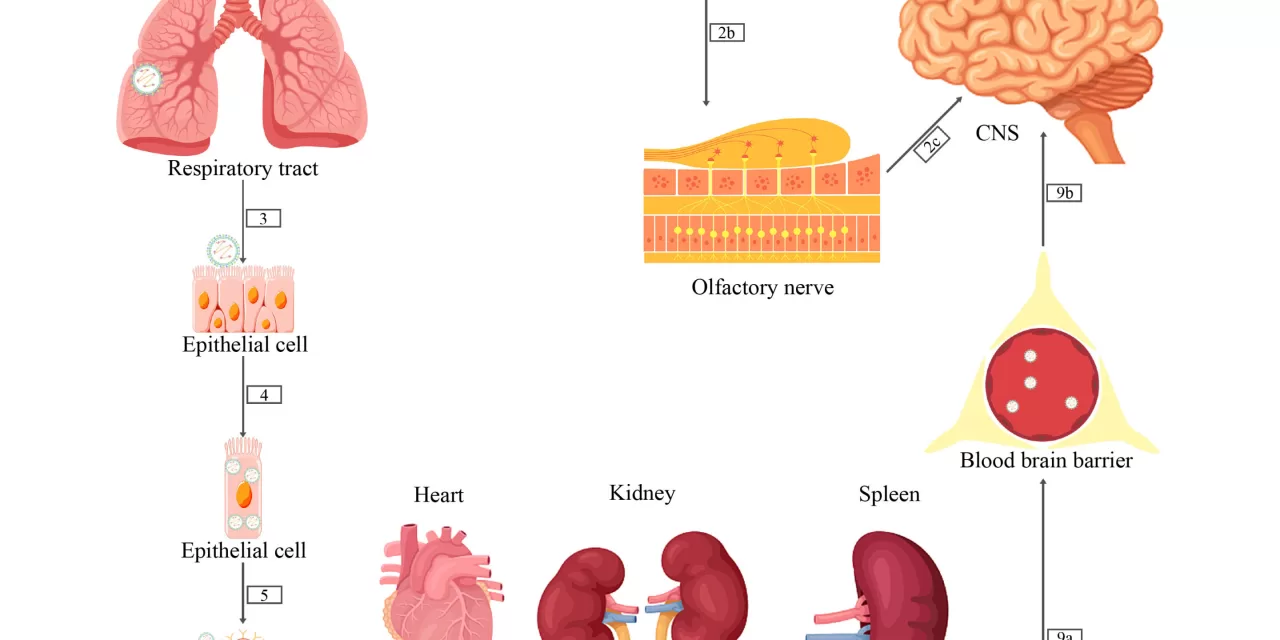
Upon infection, the virus initially targets the respiratory tract before spreading to other organs. The infection often leads to severe neurological complications, including encephalitis, a dangerous inflammation of the brain. The virus can evade the immune response, causing endothelial cell damage and contributing to its high pathogenicity. Early symptoms may resemble those of influenza, but the disease can progress rapidly, resulting in coma or death for many individuals.
Survivors face an increased risk of relapse and late-onset encephalitis, which adds to the complexity of managing NiV outbreaks. In the absence of a specific antiviral treatment, medical care is focused on supportive measures. While ribavirin has been tried as a treatment, its effectiveness remains uncertain, with research producing mixed results from in vitro studies and animal models.
Progress in Vaccine Development and Preventive Measures
Although there is currently no approved vaccine for NiV, several vaccine candidates are under development, including virus-like particle-based and mRNA-based vaccines. The need for a safe and effective vaccine is critical, especially considering the recurring outbreaks and the virus’s potential for large-scale transmission.
In the meantime, preventing NiV transmission relies on a combination of public health interventions. These include surveillance, community education, and changes in agricultural practices, such as controlling bat access to date palm sap, which has been a source of human infections, and ensuring rigorous hygiene in pig farming. The review calls for increased efforts to reduce human exposure and improve early detection to prevent outbreaks.
The Way Forward
The review underscores the importance of a multidisciplinary approach to tackling the threat posed by NiV. Enhanced global collaboration, investment in research, and the development of effective therapeutics and vaccines are essential to curb the spread of the virus. As NiV continues to emerge in new regions, the public health community must remain vigilant, prepared to respond quickly and effectively to prevent further loss of life.
For more information, refer to the article “Nipah virus: epidemiology, pathogenesis, treatment, and prevention,” by Limei Wang et al., published in Frontiers of Medicine (2024). DOI: 10.1007/s11684-024-1078-2.