Boston, MA – A new analysis by researchers at Beth Israel Deaconess Medical Center (BIDMC) has found that Vitamin D supplementation does not reduce the risk of cardiovascular disease (CVD), even among older adults with low Vitamin D levels. The study, recently published in the American Journal of Preventative Cardiology, challenges the idea that taking Vitamin D supplements can lower the risk of heart-related issues, despite previous observational studies suggesting a link between Vitamin D deficiency and cardiovascular disease.
Cardiovascular disease remains the leading cause of death for adults over the age of 65, and many seniors also exhibit low levels of Vitamin D, a nutrient thought to play a role in heart health. However, results from this randomized, double-blind trial, the gold standard in medical research, revealed no evidence that higher doses of Vitamin D supplementation reduced markers of cardiac injury or strain.
Study Details and Findings
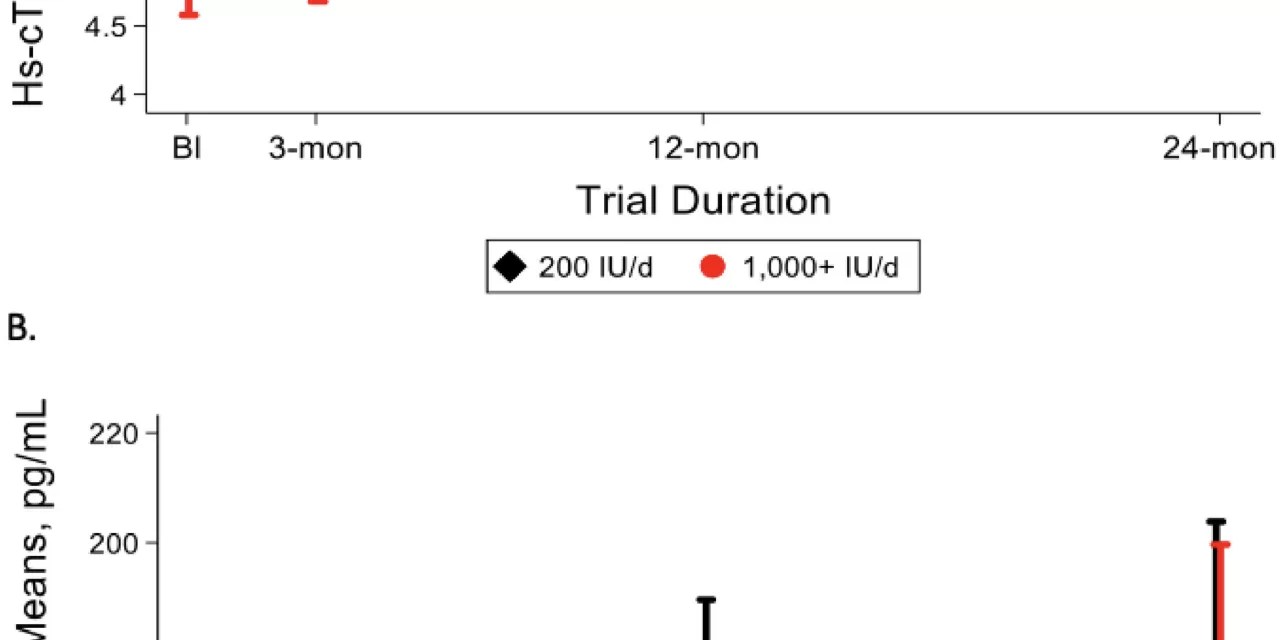
The BIDMC study analyzed data from the Study to Understand Fall Reduction and Vitamin D in You (STURDY), a National Institute of Aging-sponsored trial conducted from 2015 to 2019. The STURDY trial originally aimed to assess Vitamin D3’s impact on fall prevention in adults aged 70 or older with low Vitamin D levels. As part of the study, participants were randomly assigned to receive either 200, 1000, 2000, or 4000 international units (IU) of Vitamin D3 daily. Researchers monitored two specific blood proteins known to indicate cardiac injury and strain, with blood samples collected at baseline, three months, one year, and two years into the study.
“While multiple observational studies have demonstrated a relationship between low Vitamin D and high cardiovascular disease risk, few randomized controlled trials have directly tested whether supplementation can reduce this risk,” explained Dr. Katharine W. Rainer, the study’s lead author and a resident physician at BIDMC. “Our study decisively showed that Vitamin D had no effect on the markers of cardiovascular disease over the two-year follow-up period, regardless of dose.”
Implications and Broader Findings
The study’s findings remained consistent across various participant demographics, including age, sex, race, and pre-existing conditions such as high blood pressure or diabetes. Despite lower Vitamin D levels being associated with an initial elevation in one marker of cardiovascular disease, the supplementation failed to produce a protective effect.
“While much work is needed to understand why Vitamin D deficiency is linked to CVD, our study adds to the growing body of evidence that daily or monthly supplementation does not prevent cardiovascular events or reduce markers of subclinical cardiac injury or strain,” said Dr. Stephen P. Juraschek, the study’s senior author and Research Director of the Hypertension Center at BIDMC.
Dr. Juraschek also pointed to the potential for other lifestyle factors, such as outdoor physical activity, to play a more critical role in preventing heart disease than Vitamin D supplementation. “There may be other factors upstream to Vitamin D and CVD that could be better targets for preventive interventions,” he suggested.
The results of this study may encourage a shift in focus toward these other factors when considering cardiovascular disease prevention strategies, especially for older adults.
Reference:
Katharine W. Rainer et al, “Effects of vitamin D supplementation on cardiac biomarkers: Results from the STURDY trial,” American Journal of Preventive Cardiology (2024). DOI: 10.1016/j.ajpc.2024.100871.