New research indicates that the HPV vaccine is effectively preventing cancer in men, though fewer boys than girls are receiving the vaccine in the United States.
The HPV vaccine was initially developed to prevent cervical cancer in women and has been credited, along with screening, for reducing cervical cancer rates. While evidence that the vaccine prevents HPV-related cancers in men has been slower to emerge, recent studies suggest that vaccinated men have fewer cancers of the mouth and throat compared to their unvaccinated counterparts. These cancers are over twice as common in men than in women.
In a large healthcare dataset, researchers compared 3.4 million people of similar ages, with half vaccinated and half unvaccinated. As expected, vaccinated women had a lower risk of developing cervical cancer within at least five years of getting the shots. The benefits for men were also significant, with vaccinated men showing a lower risk of developing any HPV-related cancer, including cancers of the anus, penis, mouth, and throat.
The study observed that 57 HPV-related cancers occurred among unvaccinated men—mostly head and neck cancers—compared to 26 among vaccinated men.
“We think the maximum benefit from the vaccine will actually happen in the next two or three decades,” said Dr. Joseph Curry, a head and neck surgeon at the Sidney Kimmel Cancer Center in Philadelphia and co-author of the study. “What we’re showing here is an early wave of effect.”
The findings, along with those of a second study, were released Thursday by the American Society of Clinical Oncology and will be discussed at its annual meeting next month in Chicago. The second study highlights rising vaccination rates but shows that males lag behind females in getting the HPV shots.
HPV, or human papillomavirus, is common and spread through sex. Most HPV infections cause no symptoms and clear up without treatment, but some develop into cancer, leading to about 37,000 cases annually in the United States, according to the Centers for Disease Control and Prevention (CDC).
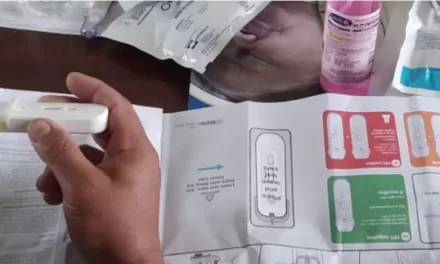
In the U.S., the HPV vaccine has been recommended since 2006 for girls aged 11 or 12, and since 2011 for boys of the same age. Catch-up shots are recommended for anyone up to age 26 who hasn’t been vaccinated.
The second study examined self- and parent-reported HPV vaccination rates among preteens and young adults from a large government survey. From 2011 to 2020, vaccination rates rose from 38% to 49% among females and from 8% to 36% among males.
“HPV vaccine uptake among young males increased by more than fourfold over the last decade, though vaccination rates among young males still fall behind females,” said Dr. Danh Nguyen of the University of Texas Southwestern Medical Center in Dallas, co-author of the study.
Jasmin Tiro of the University of Chicago Medicine Comprehensive Cancer Center, who was not involved in the research, emphasized the importance of vaccination for both boys and girls. “HPV vaccines lower cancer risk,” she said, adding that young men who haven’t been vaccinated can still get the shots.
“It’s really important that teenagers get exposed to the vaccine before they’re exposed to the virus,” Tiro said.
This new research underscores the critical need for increased HPV vaccination rates among boys to protect against HPV-related cancers and ensure long-term health benefits for both sexes.