Stanford Researchers Develop Innovative Approach to Treat Depression and Obesity
In a promising breakthrough, U.S. researchers have developed a novel form of problem-solving therapy that improves brain function and significantly alleviates symptoms of depression. The new therapy, pioneered by a team at Stanford Medicine, offers renewed hope for millions affected by this debilitating condition.
Depression, a prevalent mental health disorder, affects approximately 5% of adults worldwide. The condition is often more severe in individuals who also suffer from obesity, as both issues can impair cognitive functioning and complicate treatment.
The Stanford study, published in Science Translational Medicine, focused on 108 adults diagnosed with both major depression and obesity—a combination that often signifies challenges within the brain’s cognitive control circuit. The participants were split into two groups, with 59 individuals undergoing a year-long problem-solving therapy program in addition to their usual medical care, and 49 receiving only standard care such as medication and visits to a primary care physician.
The results were encouraging: 32% of those in the therapy group experienced a dramatic reduction in depression symptoms, with severity levels cut in half. This is a significant improvement compared to the typical 17% response rate for antidepressants among patients with both depression and obesity.
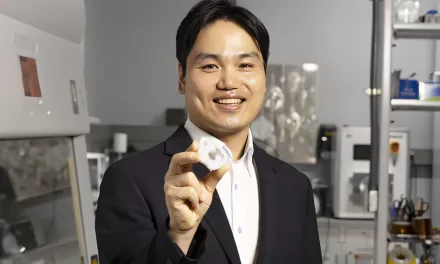
Lead author Xue Zhang, a postdoctoral scholar in psychiatry at Stanford, described the findings as “a huge improvement,” especially for patients who have traditionally been difficult to treat. Zhang explained that the therapy worked by enhancing the brain’s ability to process information efficiently, particularly in areas related to problem-solving and cognitive control.
Participants in the study underwent fMRI brain scans and completed questionnaires to assess their problem-solving skills and depression symptoms. The brain scans revealed that individuals in the standard care group experienced decreased activity in their cognitive control circuits over time, which correlated with worsening problem-solving abilities. However, in the group receiving problem-solving therapy, the reverse pattern was observed—reduced activity in the cognitive control circuit was linked to improved problem-solving capabilities.
Researchers believe the therapy helps the brain “work smarter,” allowing patients to process information more effectively. “While before the therapy, their brains had been working harder, now, they were working smarter,” Zhang and her team noted.
The therapy not only reduced depression severity but also led to noticeable improvements in daily functioning for some participants. Many reported being able to return to work, resume hobbies, and manage social interactions more effectively. These gains highlight the potential of problem-solving therapy to restore quality of life for those struggling with both depression and obesity.
This study represents a major step forward in treating hard-to-manage depression and suggests that cognitive therapies like problem-solving may offer new avenues for patients who have not responded well to traditional antidepressants.
As researchers continue to refine this approach, millions of people worldwide may soon benefit from a therapy that boosts brain function and helps them overcome the complex challenges of depression.