Albany, U.S. – Severe sepsis, a life-threatening condition triggered by bacterial or viral infections, poses a persistent challenge to medical professionals due to its potential long-term effects on the immune system. A recent study led by Katherine MacNamara and her team from Albany Medical College sheds light on the mechanisms underlying this immune suppression, offering new avenues for treatment. Their findings were published in the journal Stem Cell Reports.
Sepsis-induced immune suppression can render individuals more susceptible to recurrent infections, significantly impacting their quality of life and posing a grave risk to their health. Despite its clinical significance, the precise causes of this immune dysregulation have remained elusive, hampering the development of effective treatments.
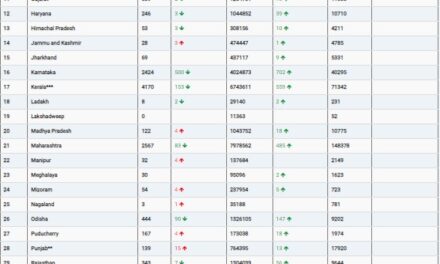
The researchers focused on understanding how severe sepsis affects blood stem cells, crucial players in the body’s immune response, residing in the bone marrow. During acute infection, these stem cells are activated by inflammatory signaling molecules known as cytokines. This activation prompts them to proliferate and migrate into the bloodstream, where they generate immune cells essential for combating the infection. However, once the infection is cleared, cytokine levels return to normal, halting the activation of blood stem cells and the production of immune cells.
The study delved into how this process is disrupted in individuals recovering from severe sepsis. Analyzing the blood stem cells of mice with prior sepsis, the researchers made a surprising discovery. Despite appearing fully recovered and functional in the bone marrow, the blood stem cells of sepsis survivors exhibited a critical impairment. Upon exposure to a second round of inflammatory stimulation, mimicked using a stem cell mobilizing agent called G-CSF, these stem cells failed to undergo the expected activation and mobilization observed in mice without prior sepsis.
As a consequence, immune cells were not efficiently produced in mice with a history of sepsis, likely contributing to their increased vulnerability to secondary infections. These findings provide valuable insights into why treatments involving inflammatory cytokines and G-CSF have shown limited efficacy in sepsis patients during clinical trials.
“This study highlights the importance of understanding the long-term consequences of severe sepsis on the immune system,” remarked Katherine MacNamara, the lead researcher. “Our findings suggest that targeting the dysregulated response of blood stem cells could hold promise for developing new therapies to combat post-sepsis immune suppression.”
The study’s implications extend beyond the realm of sepsis, offering potential insights into immune dysregulation in other conditions and paving the way for novel therapeutic strategies. By elucidating the intricate interplay between inflammatory signaling and blood stem cell function, this research represents a significant step forward in the quest to mitigate the devastating effects of severe sepsis on the immune system.
The publication of this study, titled “Survivors of Polymicrobial Sepsis are Refractory to G-CSF-Induced Emergency Myelopoiesis and Hematopoietic Stem and Progenitor Cell Mobilization,” marks a crucial milestone in the ongoing efforts to unravel the complexities of post-sepsis immune suppression and develop targeted interventions to improve patient outcomes.