This current Disease Outbreak News on the multi-country monkeypox outbreak is an update to the previously published Disease Outbreak News of 4 June, with updated data, some further detail on clinical description of cases, measures to increase the safety of gatherings, and again provides summaries of guidance, including on vaccination.
Outbreak at a glance
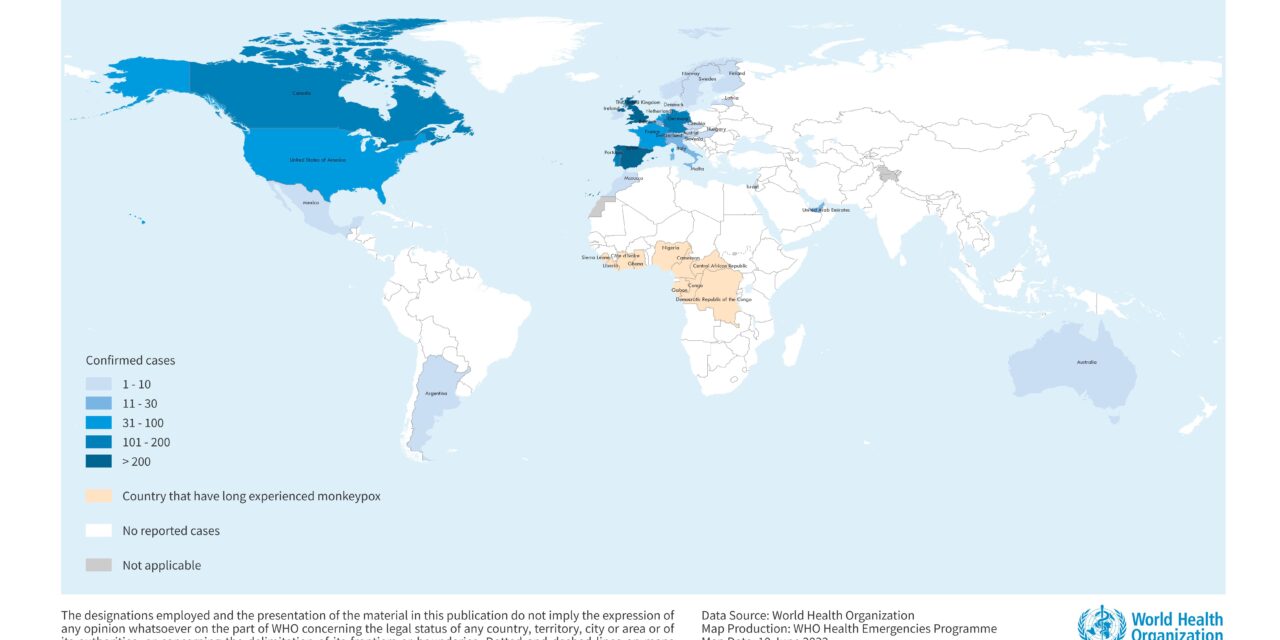
Since 13 May 2022, cases of monkeypox have been reported to WHO from 28 Member States across four WHO regions (the Region of the Americas as well as the European, Eastern Mediterranean, and Western Pacific Regions) where monkeypox is not usual or has not previously been reported (Figure 1). In addition, since the beginning of the year, there are 1536 suspected cases reported from eight countries in the WHO African Region, of which 59 cases have been confirmed and 72 deaths reported.
The continuous detection of the virus and deaths reported in some countries in the African Region highlight the need to better understand the source, transmission dynamics and provide people with the information and support they need to protect themselves and others in a range of different contexts.
While epidemiological investigations are ongoing, most reported cases in the newly affected countries have presented through sexual health or other health services in primary or secondary health care facilities with travel history to countries in Europe and North America rather than to countries where the virus is known to be present. In the countries that have long experienced monkeypox, more analysis is needed to understand the ongoing and new sources of infection.
The sudden and unexpected appearance of monkeypox simultaneously in several regions without direct immediate travel links to areas that have long experienced monkeypox suggests that there may have been undetected transmission for several weeks or longer.
WHO assesses the risk at the global level as moderate considering this is the first time that many monkeypox cases and clusters are reported concurrently in many countries in widely disparate WHO geographical areas.
Description of the outbreak
As of 8 June, 1285 laboratory confirmed cases and one probable case have been reported to WHO from 28 countries in four WHO Regions where monkeypox is not usual or had not previously been reported. This represents an increase of 505 laboratory confirmed cases since the previous Disease Outbreak News on 4 June 2022 when 780 cases were reported. As of 8 June 2022, there have been no associated reported deaths in these four Regions.
Of the cases reported in these regions, the majority (87%) of confirmed cases are from the WHO European Region (1112). Confirmed cases have also been reported from the Region of the Americas (153), Eastern Mediterranean Region (14) and Western Pacific Region (6). The case count fluctuates as more information is reported and becomes available daily and data is verified under the International Health Regulations (IHR 2005) (Table 1).
To date, the clinical presentation of monkeypox cases associated with this outbreak has been variable. Many cases in this outbreak are not presenting with the classically described clinical picture for monkeypox (fever, swollen lymph nodes, followed by rash concentrated on the face and extremities). Atypical features described include: presentation of only a few lesions or even just a single lesion; lesions that begin in the genital or perineal/perianal area and do not spread further; lesions appearing at different (asynchronous) stages of development; and the appearance of lesions before the onset of swollen lymph nodes, fever, malaise or other symptoms. The modes of transmission during sexual contact remain unknown; while it is known that close physical contact can lead to transmission, it is not clear what role sexual bodily fluids, including semen and vaginal fluids, play in the transmission of monkeypox.
The situation is evolving and WHO expects that there will be more cases of monkeypox identified as surveillance expands in all regions and countries.
Figure 1. Geographic distribution of cases of monkeypox reported to or identified by WHO from official public sources, between 13 May and 8 June 2022, 5 PM CEST
Table 1. Cases of monkeypox in countries where monkeypox is not usually or had not previously been reported, 13 May to 8 June 2022, 5 PM CEST
In addition to the cases reported from or identified in newly affected countries, WHO continues to receive updates on the status of ongoing monkeypox outbreaks and newly reported cases in countries [1] in the African Region through established surveillance mechanisms (including Integrated Disease Surveillance and Response). Since the beginning of 2022, 1536 suspected cases with 72 deaths were reported from eight countries as of 8 June 2022; 59 confirmed cases were reported from six countries during this same period (Table 2). This now includes cases from Ghana that had not previously reported human cases. Although an outbreak of monkeypox in the United States of America in 2003 was linked to small mammals which been imported from Ghana. Laboratory strengthening in countries that have long experienced monkeypox is a priority to enable confirmation of suspected cases.
The case fatality ratio seen in the African Region underlines the need for support for all elements of the response including but not limited to, awareness-raising, risk communication, surveillance, diagnostic and laboratory support, and research and analysis in the Region. WHO is providing guidance and reporting forms to countries that have long experienced monkeypox as well as countries that have newly been affected.
Table 2. Cases of monkeypox in WHO African Region reported since January 2022, as of 8 June 2022 [1]
[1] For additional information please refer to WHO AFRO Weekly Bulletin on Outbreaks and Other Emergencies here
Public health response
WHO continues to support sharing of information. Clinical and public health incident response has been activated to coordinate comprehensive case finding, contact tracing, laboratory investigation, clinical management, isolation, and implementation of infection prevention and control measures. Genomic sequencing of viral DNA, where available, is being undertaken. Several European countries (Belgium, Finland, France, Germany, Israel, Italy, the Netherlands, Portugal, Slovenia, Spain, Switzerland, the United Kingdom of Great Britain and Northern Ireland) and the United States of America have published full-length or partial genome sequences of the monkeypox virus found in the current outbreak. While investigations are ongoing, preliminary data from polymerase chain reaction (PCR) assays indicate that the monkeypox virus genes detected belong to the West African clade. Two types of vaccines (ACAM-2000 and MVA-BN) are being deployed by some Member States to serve as prophylaxis for close contacts. Others may hold supplies of other types of vaccines (e.g., LC16).
Interim guidance is being or has been developed to support Member States with raising awareness, surveillance, laboratory diagnostics and testing, case investigation and contact-tracing, clinical management and infection prevention control, vaccines and immunization, and risk communication and community engagement.
WHO has developed the following documents:
Information for the public and groups at risk
- Monkeypox: what you need to know (2 June 2022)
- Monkeypox outbreak: update and advice for health workers (26 May 2022)
- Monkeypox: public health advice for gay, bisexual and other men who have sex with men (MSM) (25 May 2022)
- Monkeypox Q&A (20 May 2022)
Technical guidance for countries
- Clinical management and infection prevention and control for monkeypox (10 June 2022)
- Monkeypox minimum dataset case reporting form (CRF) (4 June 2022)
- Interim advice on Risk Communication and Community Engagement during the monkeypox outbreak in Europe, 2022 (2 June 2022)
- Technical brief (Interim) and priority actions: Enhancing readiness for monkeypox in WHO South-East Asia Region (28 May 2022)
- Laboratory testing for the monkeypox virus: Interim guidance (23 May 2022)
- Surveillance, case investigation and contact tracing for monkeypox: Interim guidance (22 May 2022)
- Monkeypox outbreak toolbox (updated June 2022)
Documents under development (for more information see WHO Advice section below)
- Vaccines and immunization for monkeypox
- Public health advice for gatherings during the current monkeypox outbreak
- Homecare infographic for monkeypox patients
- Interim risk communication and community engagement guidance for the multi-country monkeypox outbreak
WHO risk assessment
Currently, the public health risk at the global level is assessed as moderate considering this is the first time that monkeypox cases and clusters are reported concurrently in many countries in widely disparate WHO geographical areas and without known epidemiological links to countries where monkeypox has been reported for many years. Cases have mainly, but not exclusively, been identified amongst men self-identified as part of extended sexual networks. The sudden appearance and wide geographic scale indicate that widespread human-to-human transmission is underway, for the time being still primarily in one demographic and social group, and the virus may have been present and undetected for several weeks or longer. Additionally, there is currently limited epidemiological and laboratory information, and the actual number of cases is likely an underestimate. This may in part be due to the lack of early clinical recognition of an infection previously known to occur mostly in West and Central Africa, limited surveillance and a lack of rapid diagnostics.
At present transmission in newly affected countries is primarily linked to recent sexual contacts. There is a high likelihood that further cases will be found without identified chains of transmission, including potentially in other population groups. Given the number of countries across several WHO regions reporting cases of monkeypox, it is highly likely that other countries will identify cases and there will be further spread of the virus. Human-to-human transmission occurs through close or direct physical contact with infectious lesions or mucocutaneous sores (through face-to-face, skin-to-skin, mouth-to-mouth, mouth-to-skin transmission) including during sexual activity, respiratory droplets (and possibly short-range aerosols), or contact with contaminated materials (e.g., linens, bedding and clothing).
Although the current risk to human health and to the general public remains low, the public health risk would be greater if this virus exploits the opportunity to establish itself as a widespread human pathogen. There is also a risk to health workers if they are not wearing appropriate personal protective equipment (PPE) to prevent contracting an infection; though not reported in this current outbreak, the risk of health care-associated infections has been documented in the past. There is the potential for increased health impact with wider dissemination in vulnerable groups, as the risk of severe disease and mortality is recognized to be higher among children and immunocompromised individuals, including persons with poorly controlled HIV. Infection with monkeypox in pregnancy is poorly understood, although limited data suggests that infection may lead to adverse outcomes for the foetus or newborn infant.
To date, all cases identified in newly affected countries whose samples were confirmed by PCR have been identified as being infected with the West African clade. There are two known clades of monkeypox, one identified in West Africa (WA) and one in the Congo Basin (CB) region. The WA clade has in the past been associated with overall lower mortality fewer than one in a hundred cases while the CB clade appears to cause more severe disease with a case fatality ratio (CFR) previously reported of up to one in ten; both estimates are based on infections among a generally younger population in the African setting.
Vaccination against smallpox was shown in the past to be cross-protective against monkeypox. However, any immunity from smallpox vaccination will only be present in persons over the age of 42 to 50 years or older, depending on the country, since smallpox vaccination programmes ended worldwide in 1980 after the eradication of smallpox. The original (first generation) smallpox vaccines from the eradication programme are no longer available to the general public. In addition, protection for those who were vaccinated may have waned over time.
Smallpox and monkeypox vaccines, where available, are being deployed in a limited number of countries to manage close contacts. While smallpox vaccines have been shown to be protective against monkeypox, one vaccine exists that is approved for prevention of monkeypox. This vaccine is based on a strain of vaccinia virus (known generically as modified vaccinia Ankara Bavarian Nordic strain, or MVA-BN). This vaccine has been approved for prevention of monkeypox in Canada and the United States of America. In the European Union, this vaccine has been approved for prevention of smallpox under exceptional circumstances. An antiviral to treat orthopoxviruses, tecovirimat, has been approved by the European Medicines Agency, the United States Food and Drug Administration and Health Canada. WHO has convened experts to review the latest data on smallpox and monkeypox vaccines, and to provide guidance on how and in what circumstances they should be used.
WHO advice
The advice provided hereafter by the WHO on actions required to respond to the multi-country monkeypox outbreak, is based on its technical work, and informed by frequent consultations with the following existing WHO advisory bodies: the Strategic and Technical Advisory Group on Infectious Hazards (STAG-IH); the ad-hoc Strategic Advisory Group of Experts on Immunization (SAGE) working group on smallpox and monkeypox vaccines; the Emergencies Social Science Technical Working Group; the Advisory Committee on Variola Virus Research; WHO Research & Development (R&D) Blueprint consultation: monkeypox research; the Scientific Advisory Group for the Origins of Novel Pathogens (SAGO); as well as by the outcome of ad-hoc meetings of experts.
All countries should be on the alert for signals related to patients presenting with a rash that progresses in sequential stages – macules, papules, vesicles, pustules, scabs, at the same stage of development or over all affected areas of the body – that may be associated with fever, enlarged lymph nodes, back pain, and muscle aches. During this current outbreak, many individuals are presenting with localized rash that may be in different stages of development (which is atypical for monkeypox) with peri-genital and/or peri-anal distribution associated with local, painful swollen lymph nodes. Some cases may have secondary bacterial infections, including sexually transmitted infections. These individuals may present to various community and health care settings including but not limited to primary and secondary care, fever clinics, sexual health services, infectious disease units, obstetrics and gynaecology, emergency departments, and dermatology clinics.
Increasing awareness among potentially affected communities, as well as health care providers and laboratory workers, is essential for identifying and preventing further cases and effective management of the current outbreak.
Any individual meeting the definition for a suspected case should be offered testing. The decision to test should be based on both clinical and epidemiological factors, linked to an assessment of the likelihood of infection. Due to the range of conditions that cause skin rashes and because clinical presentation may more often be atypical in this outbreak, it can be challenging to differentiate monkeypox solely based on the clinical presentation.
Caring for patients with suspected or confirmed monkeypox requires early recognition through screening protocols adapted to local settings, prompt, isolation and rapid implementation of appropriate infection, prevention and control (IPC) measures (standard and transmission-based precautions), physical examination of the patient, testing to confirm diagnosis, symptomatic management of patients with mild or uncomplicated monkeypox and monitoring for and treatment of complications and life-threatening conditions such as progression of skin lesions, secondary infection of skin lesions, and rarely, severe dehydration, severe pneumonia or sepsis.
Precautions (isolation) should remain in place until lesions have crusted, scabs have fallen off and a fresh layer of skin has formed underneath.
Information should reach those who need it most during upcoming small and large gatherings, particularly among social and sexual networks where there may be close, frequent or prolonged physical or sexual contact, particularly if this involves more than one partner. All efforts should be made to avoid the unnecessary stigmatization of individuals and communities potentially affected by monkeypox.
WHO is closely monitoring the situation and supporting international coordination working with Member States and partners.
For related WHO documents, please see the Public Health Response section above. Key updates from these documents and highlights from guidance under development are provided below for ease of reference.
Surveillance and reporting
An updated format of the minimum data set (formatted as a case report form) is available, as well as the WHO Monkeypox minimum dataset case reporting form (CRF) published online.
A separate Case Investigation and Contact Tracing form for Member States’ own use is currently being finalized and will be shared as soon as available.
Laboratory testing and sample management
Details can be found in Laboratory testing for the monkeypox virus: Interim guidance (23 May 2022)
Risk communication and community engagement
Communicating monkeypox-related risks and engaging at-risk and affected communities, community leaders, civil society organizations, and health care providers, including those at sexual health clinics, on prevention, detection and care, is essential for preventing further secondary cases and effective management of the current outbreak. Providing public health advice on how the disease transmits, its symptoms and preventive measures and targeting community engagement to the population groups who are most at risk, is critical to minimize spread. Communication must be direct, explicit and engaging for the intended audience.
Anyone who has direct contact (e.g., face-to-face, skin-to-skin, mouth-to-mouth, mouth-to-skin) including but not limited to sexual contact, with an infected person can get monkeypox. Steps for self-protection include avoiding sexual contact with someone with a localized anogenital rash or skin lesions and limiting the number of sex partners; avoiding close contact with someone who has symptoms consistent with possible monkeypox infection; keeping hands clean with water and soap or alcohol-based gels; and maintaining respiratory etiquette.
As the summer festival, concert and other events season is beginning in the northern hemisphere, it is important to work with event planners to ensure safe gatherings. Some settings which entail close, prolonged and frequent interactions between people may pose a higher risk of disease transmission. However, such events can be used as opportunities to conduct outreach for specific population groups with public health messaging. It is important to communicate early, often, and consistently through known and trusted communication channels and in language and terminology used by the affected populations. Public health authorities and event managers should work together to ensure targeted information reaches event-goers before, during and after the event. Working closely with community-based and civil society organizations that have direct and trusted relationships with affected populations is highly recommended.
If a person develops symptoms such as a rash with blisters on the face, hands, feet, eyes, mouth, and/or genitals and peri-anal areas; fever; swollen lymph nodes; headaches; muscle aches; and fatigue they should contact their health care provider and get tested for monkeypox. If someone is suspected or confirmed as having monkeypox, they should self-isolate, be tested, undergo clinical evaluation to assess for complications, avoid skin-to-skin and face-to-face contact with others and abstain from sex, including insertive/receptive oral, anal, vaginal sexual intercourse, until all lesions have crusted, the scabs have fallen off and a fresh layer of skin has formed underneath. (See Clinical management and infection prevention and control for monkeypox). During this period, cases can get supportive treatment to ease monkeypox symptoms. Anyone caring for a person sick with monkeypox should use appropriate personal protective measures as mentioned above. Based on the precautionary principle, WHO suggests the use of condoms consistently during sexual activity (receptive and insertive oral/anal/vaginal) for 12 weeks after recovery to prevent the potential transmission of monkeypox.
Residents and travellers to countries that have long experienced monkeypox should avoid contact with sick mammals such as rodents, marsupials, non-human primates (dead or alive) that could harbour monkeypox virus and should refrain from eating or handling wild game (bush meat).
WHO is continually updating its content through the monkeypox Q&A, public communication platforms, and other materials. Please see links in Public Health Response section above.
Infection, prevention and control in healthcare settings
Implementation of appropriate IPC measures is essential to mitigate and control transmission of monkeypox, in health care and community settings; this includes application of a hierarchy of controls (administrative, environmental and engineering controls) and the use of PPE in reducing the risk of exposure to monkeypox within health care settings.
Health workers should apply standard precautions regularly, this includes conducting a risk assessment for every patient interaction, respiratory hygiene and cough etiquette, patient placement, PPE, aseptic technique, safe injections and sharps injury prevention, environmental cleaning and disinfection, proper handling of laundry and linen, decontamination and reprocessing or reusable patient care items and equipment, and waste management.
WHO advises that transmission-based precautions be implemented for any suspected or confirmed case of monkeypox.
Clinical management and treatment
Patients with monkeypox should be given symptomatic treatment for mild symptoms such as antipyretics for fever and analgesics for pain. Skin lesions should be kept clean and adequate nutrition and rehydration is important. Patients should be counselled about signs and symptoms of complications that require urgent care.
Though uncommon, patients with monkeypox may develop severe and life-threatening complications. For example, the confluence of skin lesions is susceptible to bacterial skin and soft tissue infections such as cellulitis, abscesses, and necrotizing soft tissue infections requiring meticulous local wound care and, in some cases, antimicrobial therapy. Subcutaneous accumulation of fluid in the crusting phase may lead to intravascular depletion and shock as well as exfoliation resulting in areas of skin that may require surgical debridement and grafting. Other complications which are rare, include severe pneumonia and respiratory distress; corneal infection which may lead leading to vision loss; loss of appetite; vomiting and diarrhoea leading to severe dehydration, electrolyte abnormalities and shock; cervical lymphadenopathy leading to retropharyngeal abscess or respiratory compromise; sepsis or septic shock; and in rare cases encephalitis and death. It therefore follows that clinical care should focus on management of clinical syndrome, maintenance of nutritional and hydration status and prevention of complications and sequelae, as and when needed.
In patients with monkeypox, antivirals should be used under randomized clinical trials with collection of standardized clinical and patient outcome data to rapidly increase evidence generation on efficacy and safety. If this is not possible, antivirals may be used under expanded access protocols, such as Monitored Emergency Use of Unregistered and Investigational Interventions (MEURI). See reference for WHO R&D blueprint for additional information.
For further information, see Clinical management and infection prevention and control for monkeypox: Interim rapid response guidance, 10 June 2022
Vaccines
The goal of the global outbreak response for monkeypox is to control the outbreak, and to effectively use public health measures to prevent onward spread of the disease. Judicious use of vaccines can support this response.
One vaccine was recently approved for monkeypox. Some countries may hold smallpox vaccine products which could be considered for use according to national guidance. Vaccines may potentially be available in limited quantities through national authorities, depending on the country.
- Control of monkeypox outbreaks primarily relies on public health measures including surveillance, contact-tracing, isolation and care of patients. While smallpox vaccines are expected to provide some protection against monkeypox, clinical data are limited.
- Most interim vaccination recommendations provided here concern off-label use.
- Some countries have maintained strategic supplies of older smallpox vaccines from the Smallpox Eradication Programme (SEP) which concluded in 1980. These first-generation vaccines held in national reserves are not recommended for monkeypox at this time, as they do not meet current safety and manufacturing standards.
- Many years of research have led to the development of new and safer (second- and third-generation) vaccines for smallpox, some of which may be useful for monkeypox and one of which (MVA-BN) has been approved for the prevention of monkeypox.
- The supply of newer vaccines is limited and access strategies are under discussion.
- Based on currently assessed risks and benefits and regardless of vaccine supply, mass vaccination is not required nor recommended for monkeypox at this time.
- Human-to-human spread of monkeypox can be controlled by public health measures including early case-finding, diagnosis and care, isolation and contact-tracing.
- All decisions around immunization with smallpox or monkeypox vaccines should be by shared clinical decision-making, based on a joint assessment of risks and benefits, between a health care provider and prospective vaccinee, on a case-by-case basis.
- Post-exposure prophylaxis (PEP): For contacts of cases, PEP is recommended with an appropriate second- or third-generation vaccine, ideally within four days of first exposure (and up to 14 days in the absence of symptoms), to prevent the onset of disease.
- Pre-exposure prophylaxis is recommended for health workers at high risk of exposure, laboratory personnel working with orthopoxviruses, clinical laboratory personnel performing diagnostic testing for monkeypox, and outbreak response team members as may be designated by national public health authorities.
- Vaccination programmes should be accompanied by a strong information campaign, robust pharmacovigilance, and conduct of vaccine effectiveness studies under rigorous clinical trial protocols with standardized collection of clinical and outcome data.
One Health
Various wild mammals have been identified as susceptible to monkeypox virus in areas that have long experienced monkeypox. These include rope squirrels, tree squirrels, Gambian pouched rats, dormice, non-human primates, among others. Some species are asymptomatic, especially those suspected of being reservoirs (rodents). Other species, such as monkeys and great apes, show skin rashes typical of those found in humans. Thus far, there is no documented evidence of domestic animals or livestock being affected by monkeypox virus. There is also no documented evidence of human-to-animal transmission of monkeypox. However, there remains a hypothetical risk of human-to-animal transmission, as such appropriate measures such as physical distancing from persons with monkeypox to domestic pets, proper waste management to prevent the disease from being transmitted from infected humans to susceptible animals at home (including pets), in zoos and wildlife reserves, and also to peri-domestic animals, especially rodents.
Gatherings
Gatherings may represent a conducive environment for the transmission of monkeypox virus if they entail close, prolonged and frequent interactions among people, which in turn could expose attendees to contact with lesions, body fluids, respiratory droplets and contaminated materials. Postponing or cancelling gatherings in areas where monkeypox cases have been detected is currently not required as a default measure. The following precautionary measure can be considered to decrease risk of monkeypox transmission associated with such events:
- Event organizers should be aware of the epidemiology of monkeypox in the host area, its modes of transmission and prevention, and what action should be taken if a person develops signs and symptoms compatible with monkeypox, including where appropriate care can be sought. This information should be shared with prospective attendees and all those involved in the event planning and delivery.
- Gatherings should be used as opportunities for information outreach and community engagement; attention should also be dedicated to the social context in which the event takes place, with a focus on individual risk behaviours associated with side gatherings, unplanned congregation, and unstructured socialization in public or private spaces.
- People with signs and symptoms consistent with monkeypox should refrain from close contact with any other individual and should avoid attending gatherings. They should follow advice issued by relevant health authorities.
- Although monkeypox and COVID-19 spread between people differently, some of the COVID-19 measures applied during social gatherings, such as keeping a physical distance and practicing regular handwashing, are also effective against the transmission of monkeypox virus.
- As skin-to-skin, mouth-to-mouth and mouth-to-skin transmission during sexual activity has been frequently reported as a likely source of infection during the current monkeypox outbreak, close contact with someone who has signs and symptoms consistent with monkeypox should be avoided, including sexual contact; overall risk can be lowered by engaging in safe sexual practices, limiting the number of sexual partners, and practicing good personal hygiene. Attendance lists for participants in gatherings can be introduced, if applicable, to facilitate contact tracing if a monkeypox case is identified.
- Staff responsible for dealing with attendees who fall ill at the event should be provided with information on how to identify and manage people with signs and symptoms consistent with monkeypox.
- Risk communication and community engagement activities, as well as measures for early detection of international travelers with signs and symptoms consistent with monkeypox at points of entry should be considered in host countries where monkeypox cases have been reported.
- Attendees should always be reminded to apply individual-level responsibility to their decisions and actions, with the aim of preserving their health, that of the people they interact with, and ultimately that of their community. This is especially important for spontaneous or unplanned gatherings.
As it is standard practice for gatherings, and even more so during the COVID-19 pandemic, authorities and event organizers are invited to apply the WHO-recommended risk-based approach to decision-making, and tailor it to the large or small social events under consideration. In the context of the current outbreak, monkeypox-associated risks should be considered and factored in.
International travel and points of entry
Based on available information at this time, WHO does not recommend that States Parties adopt any international travel-related measures for either incoming or outgoing travellers.
Any individual feeling unwell, including fever with rash-like illness, or being considered a suspected or confirmed case of monkeypox by jurisdictional health authorities, should avoid undertaking any travel, including international, until declared as no longer constituting a public health risk. Any individual who has developed a rash-like illness during travel or upon return should immediately report to a health professional, providing information about all recent travel, smallpox immunization history, and information on close contacts as per WHO interim guidance on surveillance, case investigation and contact tracing for monkeypox. Individuals who have been identified as contacts of monkeypox cases and, therefore, are subject to health monitoring, should avoid undertaking any travel, including international, until completion of their health monitoring period.
Public health officials should work with travel operators and public health counterparts in other locations to contact passengers and others who may have had contact with an infectious person while travelling. Health promotion and risk communication materials should be available at points of entry, including information on how to identify signs and symptoms consistent with monkeypox; on the precautionary measures recommended to prevent its spread; and on how to seek medical care at the place of destination when needed.
WHO urges all Member States, health authorities at all levels, clinicians, health and social sector partners, and academic, research and commercial partners to respond quickly to contain local spread and, by extension, the multi-country outbreak of monkeypox. Rapid action must be taken before the virus can be allowed to establish itself as a human pathogen with efficient person-to-person transmission in areas that have long experienced monkeypox, as well as in newly affected areas.
Further information
For more information on monkeypox, please see:
WHO Guidance and Public Health Recommendations
- WHO Clinical management and infection prevention and control for monkeypox https://www.who.int/publications/i/item/WHO-MPX-Clinical-and-IPC-2022.1
- WHO Surveillance, case investigation and contact tracing for Monkeypox: Interim guidance, 22 May 2022. https://www.who.int/publications/i/item/WHO-MONKEYPOX-surveillance-2022.1
- WHO Laboratory testing for the monkeypox virus: Interim guidance, 23 May 2022. https://www.who.int/publications/i/item/WHO-MONKEYPOX-laboratory-2022.1
- WHO Monkeypox: public health advice for gay, bisexual and other men who have sex with men, 25 May 2022. https://www.who.int/news/item/25-05-2022-monkeypox–public-health-advice-for-gay–bisexual-and-other-men-who-have-sex-with-men
- WHO Monkeypox outbreak: update and advice for health workers, 26 May 2022. https://www.who.int/docs/default-source/coronaviruse/risk-comms-updates/update_monkeypox-.pdf?sfvrsn=99baeb03_1
- WHO Guidance on regulations for the transport of infectious substances 2021-2023, 25 February 2021. https://www.who.int/publications/i/item/9789240019720
- WHO Technical brief (interim) and priority actions: enhancing readiness for monkeypox in WHO South-East Asia Region, 28 May 2022. https://cdn.who.int/media/docs/default-source/searo/whe/monkeypox/searo-mp-techbrief_priority-actions_300522.pdf?sfvrsn=ae7be762_1
Resources
- WHO disease outbreak news: Monkeypox, all items related to multi-country outbreak: https://www.who.int/emergencies/emergency-events/item/2022-e000121
- WHO disease outbreak news: Monkeypox, all previous items: https://www.who.int/emergencies/emergency-events/item/monkeypox
- WHO AFRO Weekly Bulletin on Outbreaks and Other Emergencies, Epidemiological Week 21, 2022: https://apps.who.int/iris/bitstream/handle/10665/354552/OEW21-1622052022.pdf
- WHO AFRO Weekly Bulletin on Outbreaks and Other Emergencies, Week 22, 2022 https://apps.who.int/iris/bitstream/handle/10665/354782/OEW22-2329052022.pdf
- WHO factsheet on monkeypox, publishing date, 19 May 2022. http://www.who.int/news-room/fact-sheets/detail/monkeypox
- WHO Health topics – Monkeypox: https://www.who.int/health-topics/monkeypox#tab=tab_1
- WHO monkeypox outbreak tool kit. https://www.who.int/docs/default-source/documents/emergencies/outbreak-toolkit/monkeypox-toolbox-20112019.pdf?sfvrsn=c849bd8b_2
- Open WHO. Online training module. Monkeypox: Introduction. 2020 English: https://openwho.org/courses/variole-du-singe-introduction
- Open WHO. Extended training. Monkeypox epidemiology, preparedness and response. 2021.English: https://openwho.org/courses/monkeypox-introduction; Français: https://openwho.org/courses/variole-du-singe-int%C3%A9roduction
- WHO 5 moments for hand hygiene. https://www.who.int/campaigns/world-hand-hygiene-day
- WHO One health GLOBAL. https://www.who.int/health-topics/one-health#tab=tab_1
- World Organisation for Animal Health, founded as OIE: Monkeypox. https://www.oie.int/en/disease/monkeypox/
- Risk Communication and Community Engagement. Public health advice on the recent outbreak of monkeypox in the WHO European Region, 24 May 2022: https://www.euro.who.int/__data/assets/pdf_file/0004/538537/public-health-advice-monkeypox-eng.pdf Interim advice on Risk Communication and Community Engagement during the monkeypox outbreak in Europe, 2022 Joint report by WHO Regional office for Europe/ECDC 2 June 2022. https://www.euro.who.int/__data/assets/pdf_file/0009/539046/ECDC-WHO-interim-advice-RCCE-Monkeypox-2-06-2022-eng.pdf United Kingdom Health Security Agency. Monkeypox guidance. https://www.gov.uk/guidance/monkeypox
- Nigeria Centre for Disease Control. Monkeypox. https://ncdc.gov.ng/diseases/info/M and https://ncdc.gov.ng/diseases/sitreps/?cat=8&name=An%20Update%20of%20Monkeypox%20Outbreak%20in%20Nigeria
- Weekly epidemiological record (WER) no.11, 16 March 2018, Emergence of monkeypox in West Africa and Central Africa 1970-2017. http://apps.who.int/iris/bitstream/handle/10665/260497/WER9311.pdf;jsessionid=7AB72F28D04CFE6CE24996192FC478FF?sequence=1
- First draft genome sequence of Monkeypox virus associated with the suspected multi-country outbreak, May 2022 (confirmed case in Portugal). https://virological.org/t/first-draft-genome-sequence-of-monkeypox-virus-associated-with-the-suspected-multi-country-outbreak-may-2022-confirmed-case-in-portugal/799
- Belgian case of monkeypox virus linked to outbreak in Portugal. https://virological.org/t/belgian-case-of-monkeypox-virus-linked-to-outbreak-in-portugal/801
- A monkeypox virus genome from a second Belgian case. https://virological.org/t/a-monkeypox-virus-genome-from-a-second-belgian-case/807
- First French draft genome sequence of monkeypox virus, May 2022. https://virological.org/t/first-french-draft-genome-sequence-of-monkeypox-virus-may-2022/819
- Illumina whole-genome sequence of Monkeypox virus in a patient travelling from the Canary Islands to France. https://virological.org/t/illumina-whole-genome-sequence-of-monkeypox-virus-in-a-patient-travelling-from-the-canary-islands-to-france/829/7
- First German genome sequence of Monkeypox virus associated to multi-country outbreak in May 2022. https://virological.org/t/first-german-genome-sequence-of-monkeypox-virus-associated-to-multi-country-outbreak-in-may-2022/812
- First Monkeypox genome sequence from Italy. https://virological.org/t/first-monkeypox-genome-sequence-from-italy/824
- First monkeypox genome sequence from the Netherlands. https://virological.org/t/first-monkeypox-genome-sequence-from-the-netherlands/821
- Spanish draft genome sequence of Monkeypox virus related to multi-country outbreak (May 2022). https://virological.org/t/spanish-draft-genome-sequence-of-monkeypox-virus-related-to-multi-country outbreak-may-2022/825
- First 2022 monkeypox outbreak genome sequences from Slovenia. https://virological.org/t/first-2022-monkeypox-outbreak-genome-sequences-from-slovenia/841
- First Israeli whole genome sequence of monkeypox virus associated with the May 2022 multi-country outbreak. https://virological.org/t/first-israeli-whole-genome-sequence-of-monkeypox-virus-associated-with-the-may-2022-multi-country-outbreak/843
- Initial observations about putative APOBEC3 deaminase editing driving short-term evolution of MONKEYPOXV since 2017, published on 30 May 2022. https://virological.org/t/initial-observations-about-putative-apobec3-deaminase-editing-driving-short-term-evolution-of-monkeypoxv-since-2017/830
- Multicolour, multiplex real-time PCR assay for the detection of human-pathogenic poxviruses. 10.1016/j.mcp.2009.10.008
- Real-time PCR assays for the specific detection of monkeypox virus West African and Congo Basin strain DNA. 10.1016/j.jviromet.2010.07.012
- Species-specific differentiation of variola, monkeypox, and varicella-zoster viruses by multiplex real-time PCR assay.10.1016/j.jviromet.2016.07.024
- Genomic epidemiology of monkeypox virus. https://nextstrain.org/monkeypox?c=country
- Global.health data on monkeypox: Monkeypox_Public_www.global.health – Google Sheets
- BNONEWS- Monkeypox tracker: https://bnonews.com/monkeypox/
- Ministry of Health of Argentina. Health reports that the result of the PCR sample derived from the ANLIS Malbrán of the second suspected case of monkeypox was positive. 27 May 2022. Available at: https://bit.ly/3tpxLiS
- Public Health Agency of Canada (PHAC) Monkeypox: Outbreak update. 9 June. Available at: https://bit.ly/3NGdWvF
- US Centers for Disease Control and Prevention (US CDC). Monkeypox in the United States 2022: Situation Summary. 8 June 2022. Available at: https://bit.ly/3NyqwwR
- Press release from the Mexico Secretary of Health. Mexico confirms first imported case of monkeypox. 28 May 2022. Available at: https://bit.ly/3tpxLiS