Lung diseases are a leading cause of death globally, claiming millions of lives each year. Despite advances in medical science, treatment options remain limited, and the use of animal models for studying these conditions and testing new medications often falls short. However, a groundbreaking study published in ACS Applied Bio Materials offers a promising new approach: mucus-based bio-ink for 3D printing lung tissue.
The challenge of developing effective treatments for chronic lung conditions, such as chronic obstructive pulmonary disease (COPD) and cystic fibrosis, is compounded by the scarcity of donor organs for transplantation. While medications can manage symptoms, a cure remains elusive. Researchers are now turning to bioengineering to create more accurate models of human lungs, potentially offering new avenues for treatment and research.
Traditional methods for studying lung diseases often rely on animal models, which may not fully replicate the complexities of human pulmonary conditions. As a result, bioengineers are exploring lab-grown lung tissues as a more precise alternative. One such innovative approach involves 3D printing techniques designed to mimic human tissue, but developing a suitable bio-ink that supports cell growth has been a significant hurdle.
To address this challenge, Dr. Ashok Raichur and his team have developed a novel mucus-based bio-ink. They began with mucin, a component of mucus with antibacterial properties, which had not been extensively used in bioprinting. Mucin’s molecular structure includes segments that resemble epidermal growth factor, a protein known for promoting cell attachment and growth.
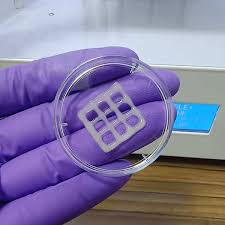
The researchers reacted mucin with methacrylic anhydride to create methacrylated mucin (MuMA), which was then combined with lung cells. They further enhanced the bio-ink by adding hyaluronic acid, a natural polymer that increases viscosity and supports cell adhesion and growth. The team printed the bio-ink into various patterns, such as round and square grids, and exposed the structures to blue light to crosslink the MuMA molecules.
This process resulted in a porous gel that absorbed water and supported cell survival. The interconnected pores in the gel facilitated nutrient and oxygen diffusion, which is crucial for cell growth and tissue formation. The printed structures proved to be nontoxic and biodegraded gradually under physiological conditions, suggesting their potential use as implants where the scaffold could be replaced by newly grown lung tissue over time.
In addition to their potential use in implants, these bio-inks could revolutionize the study of lung diseases by providing more accurate 3D models of human lungs. This could lead to better understanding of disease processes and the evaluation of new treatments.
The research was supported by the Government of India’s Department of Science and Technology, highlighting the collaborative effort driving this innovative advancement in biomedical engineering.