Introduction
The World Health Organization (WHO) recently declared a global health emergency as Mpox, previously known as monkeypox, spreads rapidly across 13 African countries, including Congo, where over 14,000 cases and 524 deaths have been reported. This article provides a detailed explainer on Mpox, an infectious disease caused by the monkeypox virus (MPXV), a member of the Orthopoxvirus genus.
Historical Context and Global Spread
Mpox was first identified in 1958 in monkeys used for research in Denmark. The first human case was reported in Congo in 1970. Following the eradication of smallpox in 1980, Mpox emerged in Central, East, and West Africa, leading to sporadic outbreaks. A significant global outbreak occurred between 2022 and 2023, primarily driven by the Clade IIb strain.
The current outbreak, now recognized as a Public Health Emergency of International Concern (PHEIC) by WHO, underscores the virus’s capacity to spread beyond endemic regions. The rapid transmission across African nations has raised alarm, with the situation in Congo being particularly severe.
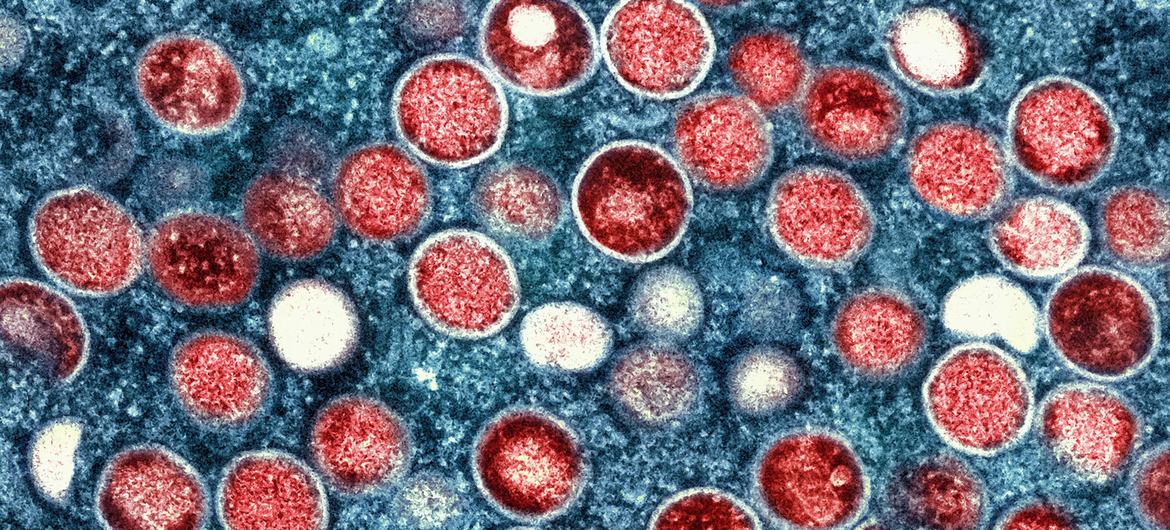
Understanding the Virus and Its Transmission
There are two distinct genetic clades of the Mpox virus: Clade I and Clade II. The disease, often characterized by painful rashes, fever, and swollen lymph nodes, spreads primarily through direct contact with infected individuals, animals, or contaminated materials.
Human-to-human transmission occurs via direct contact with infectious lesions, respiratory droplets, or contaminated objects such as bedding or clothing. Animal-to-human transmission can happen through bites, scratches, or the consumption of infected animals. The virus enters the body through broken skin, mucosal surfaces, or the respiratory tract. High-risk groups include individuals with multiple sexual partners and those in close contact with infected persons or animals.
Symptoms and Diagnosis
Symptoms of Mpox typically appear within 1-21 days after exposure and may last 2-4 weeks. The disease commonly starts with fever, muscle aches, and sore throat, followed by a rash that progresses through several stages, including macules, papules, vesicles, and pustules, before crusting over and falling off. The rash can appear anywhere on the body, including the face, mouth, genitals, and anus. Lymphadenopathy, or swollen lymph nodes, is a classic symptom of Mpox.
Diagnosing Mpox involves differentiating it from similar conditions such as chickenpox, measles, and other skin infections. Polymerase chain reaction (PCR) testing of skin lesion material is the preferred diagnostic method. Blood testing is generally not recommended, and antibody detection methods may not be useful in distinguishing Mpox from other orthopoxviruses.
Treatment and Prevention
Treatment for Mpox focuses on supportive care to manage symptoms and prevent complications. Vaccination, especially for high-risk groups such as healthcare workers and men who have sex with men, is recommended to prevent infection. Several antivirals, such as tecovirimat, originally developed for smallpox, have been used to treat Mpox, with further studies ongoing.
Preventing the spread of Mpox involves avoiding close contact with infected individuals, practicing good hygiene, and isolating infected persons until they are no longer contagious. Vaccination within four days of exposure can help prevent infection, and condoms can reduce but not eliminate the risk of transmission.
Conclusion
Mpox remains a significant global health concern due to its potential for severe complications, particularly in children, pregnant individuals, and those with weakened immune systems. Continued surveillance, vaccination, and public health efforts are crucial to controlling and preventing future outbreaks. The recent surge in cases across Africa highlights the need for a coordinated global response to contain this emerging epidemic.