On 25 May 2021, the United Kingdom of Great Britain and Northern Ireland notified the WHO of one laboratory-confirmed case of monkeypox. The patient arrived in the United Kingdom on 8 May 2021. Prior to travel, the patient had lived and worked in Delta State, Nigeria.
On arrival in the United Kingdom, the patient remained in quarantine with family due to COVID-19 restrictions. On 10 May, the patient developed a rash, beginning on the face. The patient remained in self-isolation for a further ten days and sought medical care for relief of symptoms. The patient was admitted to a referral hospital on 23 May. Skin lesion samples were received at the Public Health England Rare and Imported Pathogens Laboratory on 24 May. The West African clade of monkeypox virus was confirmed by polymerase chain reaction (PCR) on 25 May.
On 29 May, a family member with whom the patient quarantined developed lesions clinically compatible with monkeypox and was immediately isolated in an appropriate facility. Monkeypox was confirmed on 31 May. Both patients are stable and recovering.
Public health response
The health authorities of the United Kingdom activated an incident management team and implemented public health measures, including isolation of the index case and secondary case and contact tracing of all close contacts in the hospital and community.
Follow up is being undertaken for the contacts of the two cases for 21 days after their last exposure. No close contacts have travelled outside the United Kingdom following exposure. Post-exposure vaccination was not offered to contacts.
Information was shared with the Nigerian National IHR Focal Point who have initiated an outbreak investigation and are gathering further information regarding potential source of infection and exposures in Nigeria.
WHO risk assessment
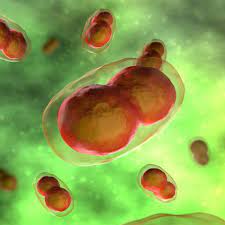
Monkeypox is a sylvatic zoonosis with incidental human infections that usually occur sporadically in forested parts of Central and West Africa. It is caused by the monkeypox virus and belongs to the Orthopoxvirus family. Monkeypox can be transmitted by contact and droplet exposure via exhaled large droplets. The incubation period of monkeypox is usually from 6 to 13 days but can range from 5 to 21 days. The disease is often self-limiting with symptoms usually resolving spontaneously within 14-21 days. Symptoms can be mild or severe, and lesions can be very itchy or painful. Milder cases of monkeypox may go unreported and represent a risk of person-to-person transmission. The animal reservoir remains unknown, although is likely to be among rodents. Contact with live and dead animals through hunting and consumption of wild game or bush meat are known risk factors.
There are two clades of monkeypox virus, the West African clade and Congo Basin (Central African) clade. Although the West African clade of monkeypox virus infection sometimes leads to severe illness in some individuals, disease is usually self-limiting. The case fatality ratio for the West African clade has been documented to be around 1% whereas for the Congo Basin clade it may be as high as 10%.
Currently in the United Kingdom, including these two cases, there have been only six cases of monkeypox reported, including three previously imported cases from Nigeria, two in September 2018 and one in December 2019. Prior to this report, there was also one case of nosocomial transmission in a health worker in England in 2018 due to contact with contaminated bed linen. In the present case, the first patient was under quarantine with family members due to COVID-19 restrictions for a period of ten days after arrival in the country and an additional two days. Contacts possibly exposed are being monitored. Once monkeypox was suspected, authorities in the United Kingdom promptly initiated appropriate public health measures, including isolation of the case and contact tracing. The second individual was isolating at home until onset of the rash and in hospital care thereafter. The risk of potential onward spread in the country is minimized.
In 2017, Nigeria began to experience its first outbreak in 40 years. From the first cases in September 2017 to November 2019, a total of 183 confirmed cases and 9 deaths were recorded in 18 states (Rivers, Bayelsa, Cross River, Imo, Akwa Ibom, Lagos, Delta, Bauchi, Federal Capital Territory (FCT), Abia, Oyo, Enugu, Ekiti, Nasarawa, Benue, Plateau, Edo, Anambra). The outbreak occurred primarily in southern parts of the country including Delta State. Public health measures included enhanced surveillance and health worker training, as well as isolation of cases, contact-tracing and quarantine. Since then, sporadic cases have continued to occur in Nigeria pointing to endemicity of the disease. In 2020, there were 14 suspected cases, three confirmed cases and no deaths. In 2021, a total of 32 suspected cases have been reported from January and May. Of the suspected cases, 7 were confirmed from five states Delta (2), Bayelsa (2), Lagos (1), Edo (1), Rivers (1) and no deaths were recorded.
While a vaccine was approved for monkeypox in 2019, and traditional smallpox vaccine provides cross-protection for monkeypox, these vaccines are not widely available. There is likely to be little immunity to the infection in those exposed as endemic disease is geographically limited to West and Central Africa. Increased susceptibility of humans to monkeypox is thought to be related to waning immunity due to cessation of smallpox immunization. Populations worldwide under the age of 40 or 50 years no longer benefit from the protection afforded by prior smallpox vaccination programmes.
Importations of monkeypox from an endemic country to another country not previously known to have cases have been documented on a total of eight, once in 2003 and the rest since 2018.
The public health risk from this reported event is low in the United Kingdom. Monkeypox remains endemic in parts of West and Central Africa and represents an ongoing risk for further local outbreaks and travel-related cases. On this occasion, the confirmed index case has a history of travel from Delta State in Nigeria, where monkeypox has previously been reported. An investigation is underway in Delta State.
WHO advice
Any illness during travel or upon return should be reported to a health professional, including information about all recent travel and immunization history. Residents and travelers to endemic countries should avoid contact with sick, dead or live animals that could harbor the monkeypox virus (rodents, marsupials, primates) and should refrain from eating or handling wild game (bush meat). The importance of hand hygiene using soap and water, or alcohol-based sanitizer should be emphasized.
A patient with monkeypox should be isolated during the infectious period, that is during the rash stage of the illness, and contacts should be observed in quarantine. Timely contact tracing, surveillance measures and raising awareness of imported emerging diseases among health care providers are essential parts of preventing secondary cases and effective management of monkeypox outbreaks.
Health-care workers caring for patients with suspected or confirmed monkeypox should implement standard, contact and droplet infection control precautions. Samples taken from people and animals with suspected monkeypox virus infection should be handled by trained staff working in suitably equipped laboratories.