Situation at a glance
From 13 September 2022 to 12 August 2023, three laboratory-confirmed cases of Middle East respiratory syndrome coronavirus (MERS-CoV), including two deaths, were reported to WHO by the Ministry of Health of the Kingdom of Saudi Arabia (KSA). Close contacts for the three cases were followed up by the Ministry of Health, and no secondary cases were identified. The notification of these cases reiterates the need for global awareness of MERS-CoV as the disease continues to pose a threat in countries where MERS-CoV is circulating in dromedary camels, including those in the Middle East.
Description of situation
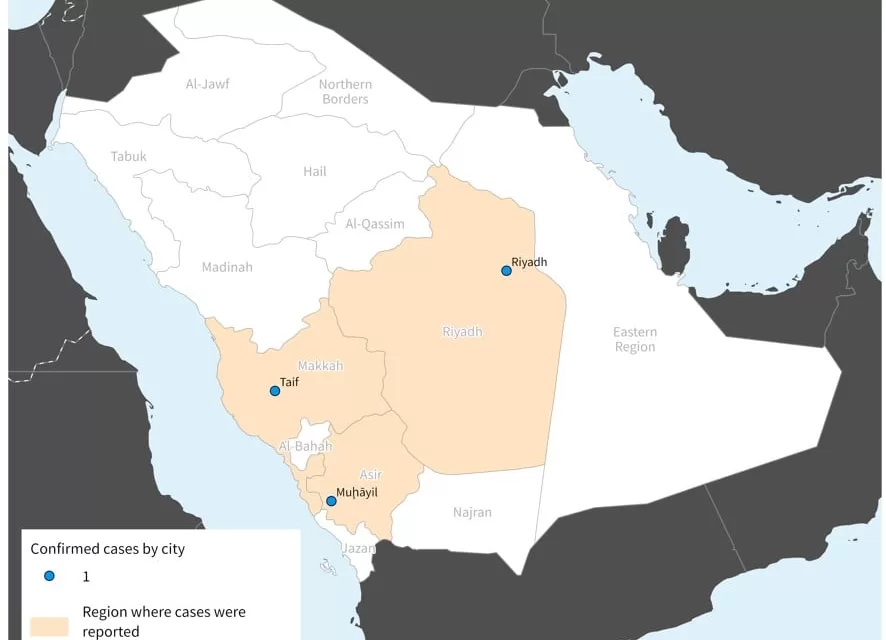
Between 13 September 2022 to 12 August 2023, the Ministry of Health of KSA reported three additional cases of Middle East respiratory syndrome coronavirus (MERS-CoV), with two associated deaths. The cases were reported from Riyadh, Asser, and Makkah Al Mukarramah regions (Figure 1). Laboratory confirmation of the cases was performed by real-time polymerase chain reaction (RT-PCR).
All three cases were non-health-care workers, who presented with fever, cough, and shortness of breath, and had comorbidities. Of the three cases, two had a history of contact with dromedary camels and all three cases had a history of consumption of raw camel milk in the 14 days prior to the onset of symptoms. All three cases were male, and aged 42, 83, and 85 years respectively (Table 1).
Since the first report of MERS-CoV in KSA in 2012, human infections have been reported from 27 countries, in all six WHO regions. Of the reported 2605 cases, the majority of MERS-CoV cases (2196; 84%) have been reported from KSA, including these newly reported cases. Of the 937 deaths reported from 27 countries, a total of 856 (91%) deaths have been reported from KSA, including the newly reported deaths (Figure 2).
Figure 1. Geographical distribution of MERS-CoV cases between 13 September 2022 and 12 August by city and region, KSA (n=3).
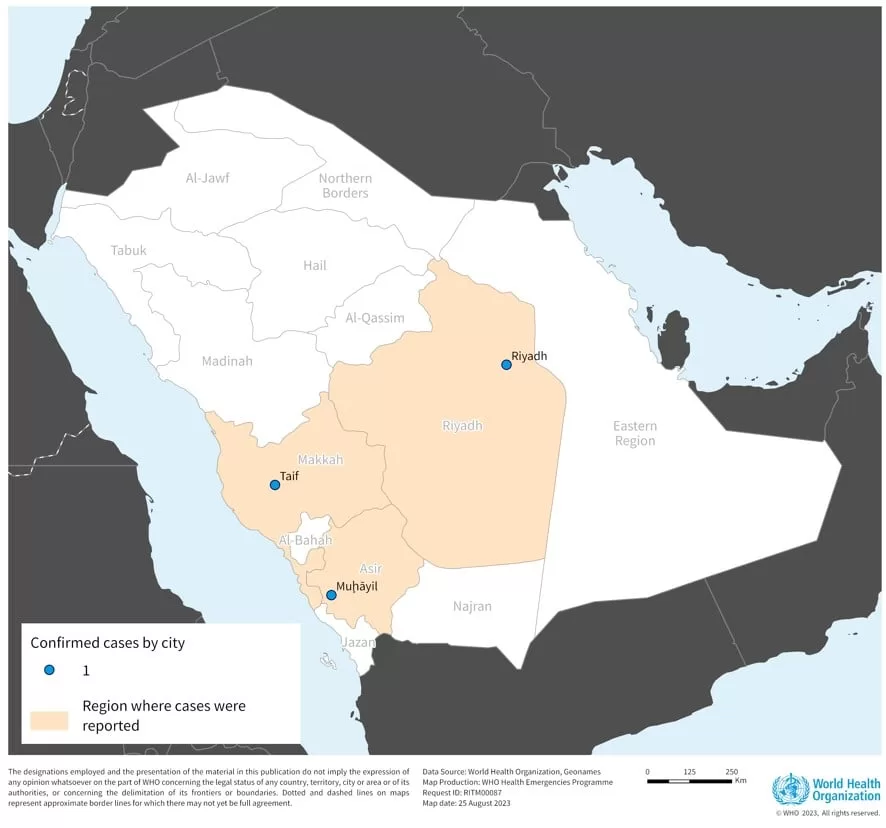
Table 1. MERS-CoV cases reported by KSA between 13 September 2022 and 12 August 2023
Figure 2: Epidemic curve of MERS-CoV cases and deaths reported in KSA between 2012 and 12 August 2023 
Epidemiology of MERS-CoV
Middle East respiratory syndrome (MERS) is a viral respiratory infection caused by the Middle East respiratory syndrome coronavirus (MERS-CoV). Approximately 36% of patients with MERS have died, though this may be an overestimate of the true mortality rate, as mild cases of MERS-CoV may be missed by existing surveillance systems, and the case fatality ratio (CFR) is calculated based only on laboratory-confirmed cases.
Humans are infected with MERS-CoV from direct or indirect contact with dromedary camels, which are the natural host and zoonotic source of the virus. MERS-CoV has demonstrated the ability to transmit between humans. So far, non-sustained human-to-human transmission has occurred among close contacts and in healthcare settings and outside of the healthcare setting, there has been limited human-to-human transmission.
MERS-CoV infections range from showing no symptoms (asymptomatic) or mild respiratory symptoms, to severe acute respiratory disease and death. A typical presentation of MERS disease is fever, cough, and shortness of breath. Pneumonia is a common finding, but not always present. Gastrointestinal symptoms, including diarrhoea, have also been reported. Severe illness can cause respiratory failure that requires mechanical ventilation and support in an intensive care unit. The virus appears to cause more severe disease in older people, persons with weakened immune systems, and those with comorbidities or chronic diseases such as renal disease, cancer, chronic lung disease, and diabetes.
No vaccine or specific treatment is currently available, although several MERS-CoV-specific vaccines and therapeutics are in development. Treatment is supportive and based on the patient’s clinical condition and symptoms.
Public health response
Follow-up of the close contacts was conducted for all three cases, and no secondary cases were identified.
For the two cases reporting contact with camels, the Ministry of Agriculture was informed, and an investigation of camels was conducted. There are no treatments available for MERS-CoV in animals. The identified positive camels were isolated until RT-PCR testing was negative.
WHO risk assessment
From 13 September 2012 to 12 August 2023, the total number of laboratory-confirmed MERS-CoV infection cases reported globally to WHO was 2605, with 937 (CFR 36%) associated deaths. The majority of these cases occurred in countries in the Arabian Peninsula, including 2196 cases with 856 related deaths (CFR 39%) in KSA. There has been one large outbreak outside of the Middle East, in the Republic of Korea, in May 2015, during which 186 laboratory-confirmed cases (185 in the Republic of Korea and 1 in China) and 38 deaths were reported. The index case in that outbreak had a travel history to the Middle East. The global number reflects the total number of laboratory-confirmed cases reported to WHO under IHR (2005) or directly by Ministries of Health. The total number of deaths includes the deaths that WHO is aware of to date through follow-up with affected Member States.
WHO expects that additional cases of MERS-CoV infection will be reported from the Middle East and/or other countries where MERS-CoV is circulating in dromedaries, and that cases will continue to be exported to other countries by individuals who were exposed to the virus through contact with dromedaries or their products (for example, consumption of raw camel milk), or in a healthcare setting. WHO continues to monitor the epidemiological situation and conducts risk assessment based on the latest available information.
The number of MERS cases reported to WHO has substantially declined since the beginning of the COVID-19 pandemic. This is likely the result of epidemiological surveillance activities for COVID-19 being prioritized and the similar clinical picture of both diseases, resulting in reduced testing and detection of MERS CoV cases. The Ministry of Health of KSA is working to improve testing capacities for better detection of MERS-CoV during the COVID-19 pandemic. In addition, measures taken during the COVID-19 pandemic to reduce SARS-CoV-2 transmission (e.g., mask wearing, hand hygiene, physical distancing, improving ventilation of indoor spaces, respiratory etiquette, stay-at-home orders, reduced mobility) also likely reduced opportunities for onward human-to-human transmission of MERS-CoV.
WHO advice
Based on the current situation and available information, WHO re-emphasizes the importance of strong surveillance by all Member States for acute respiratory infections, including MERS-CoV, and to carefully review and investigate any unusual patterns.
Human-to-human transmission of MERS-CoV in healthcare settings has been associated with delays in recognizing the early symptoms of MERS-CoV infection, slow triage of suspected cases, and delays in implementing infection, prevention, and control (IPC) measures. IPC measures are critical to prevent the possible spread of MERS-CoV between people in healthcare facilities. Healthcare workers should always apply standard precautions consistently with all patients, at every interaction in healthcare settings. Droplet precautions should be added to the standard precautions when providing care to patients with symptoms of acute respiratory infection; contact precautions and eye protection should be added when caring for probable or confirmed cases of MERS-CoV infection; airborne precautions should be applied when performing aerosol generating procedures or in settings where aerosol generating procedures are conducted. Early identification, case management and isolation of cases, quarantine of contacts, together with appropriate infection prevention and control measures in health care setting and public health awareness can prevent human-to-human transmission of MERS-CoV.
MERS-CoV appears to cause more severe disease in people with underlying chronic medical conditions such as diabetes, renal failure, chronic lung disease, and immunocompromised persons. Therefore, people with these underlying medical conditions should avoid close contact with animals, particularly dromedaries, when visiting farms, markets, or barn areas where the virus may be circulating. General hygiene measures, such as regular hand washing before and after touching animals and avoiding contact with sick animals, should be adhered to.
Food hygiene practices should be observed. People should avoid drinking raw camel milk, camel urine or eating meat that has not been thoroughly cooked. The consumption of raw or undercooked animal products, including milk and meat, carries a high risk of infection from pathogens that may cause disease in humans. Animal products that are processed appropriately through cooking or pasteurization are safe for consumption. Foods that have gone through these processes should be handled with care to avoid cross contamination with uncooked/unsafe foods. Camel meat and camel milk are nutritious products that can continue to be consumed after cooking, pasteurization or other thermal treatments.
WHO does not advise special screening at points of entry regarding this event, nor does it currently recommend the application of any travel or trade restrictions.
Further information
- MERS Fact sheet
- Middle East Respiratory Syndrome Overview
- MERS global summary and assessment of risk
- WHO EPI-WIN Update 88: MERS-CoV, a circulating coronavirus with epidemic and pandemic potential – Pandemic preparedness, prevention and response with a One Health approach
- WHO EPI-WIN webinar: MERS-CoV, a circulating coronavirus with epidemic and pandemic potential – Pandemic preparedness, prevention and response with a One Health approach
- WHO-EMRO MERS monthly bulletin
- Middle East Respiratory Syndrome Outbreak Toolbox
- MERS outbreak in the Republic of Korea, 2015
- Disease Outbreak News
- Korea Disease control and Prevention agency, Middle East Respiratory Syndrome (MERS) outbreak in 2015:
- Five keys to safer food manual.
Citable reference: World Health Organization (29 August 2023). Disease Outbreak News; Middle East respiratory syndrome coronavirus (MERS-CoV) – Saudi Arabia. Available at: https://www.who.int/emergencies/disease-outbreak-news/item/2023-DON484