Situation at a glance
From 1 November 2022 to 27 January 2023, a total of 559 cases of meningitis (of which 111 are laboratory confirmed), including 18 deaths (overall CFR 3.2%), have been reported from Zinder Region, southeast of Niger, compared to the 231 cases reported during 1 November 2021 to 31 January 2022. The majority of laboratory-confirmed cases (104/111; 93.7%) are due to Neisseria meningitidis serogroup C (NmC). Reactive vaccination campaigns with the trivalent ACW meningococcal polysaccharide vaccine have been implemented.
Niger is located largely in the African meningitis belt with seasonal outbreaks recurring every year. However, the ongoing outbreak shows both an increased number of cases and an increased growth rate compared to the previous seasons.
Zinder region shares an international border with Jigawa State in Nigeria where a NmC outbreak is also ongoing, confirming the risk of international spread. Moreover, the simultaneous occurrence of other epidemics, insecurity and population displacement, all in the context of a protracted humanitarian crisis, are likely to contribute to the spread of the outbreak in other countries of the West African subregion.
WHO assesses the risk posed by the current meningitis outbreak in Niger as high at the national level, moderate at the regional level, and low at the global level.
Description of the situation
Being located in the African meningitis belt, Niger has been affected by several meningitis epidemics resulting in 20 789 cases and 1369 deaths (CFR 6.6%) reported since 2015.
From 1 November 2022 to 27 January 2023, a total of 559 cases of meningitis (of which 111 are laboratory confirmed), including 18 deaths (overall CFR 3.2%) have been reported from Zinder region, southeast of Niger, compared to the 231 cases reported during 1 November 2021 to 31 January 2022.
The last meningitis outbreak in the Zinder region, occurred in the 2021/2022 season, with a total of 372 cases, including 12 deaths (CFR 3%).
Figure 1. Epicurve of cases of meningitis reported in Niger by month, 1 October 2021 – 27 January 2023. 
Of the 228 samples collected from suspected cases, 154 (67.5%) have been analyzed by Niamey’s Center for Medical and Health Research (CERMES). Neisseria meningitidis serogroup C was identified in the majority of confirmed cases (n=104; 93.7%), followed by Streptococcus pneumoniae (n=5; 4.5%) and Haemophilus influenzae (n=2; 1.8%). The remaining 43 samples tested negative.
Males represent 53% of all cases. Among the total of 559 cases of meningitis, people under 20 years of age are the most affected by the outbreak (n=538; 96.3%), with 202 cases (36.2%) reported in the 10-14 years age group, followed by the 5-9 years age group with 153 cases (27.4%), the 15-19 years age group with 107 cases (19.1%), and the 0-4 years age group with 76 cases (13.6%).
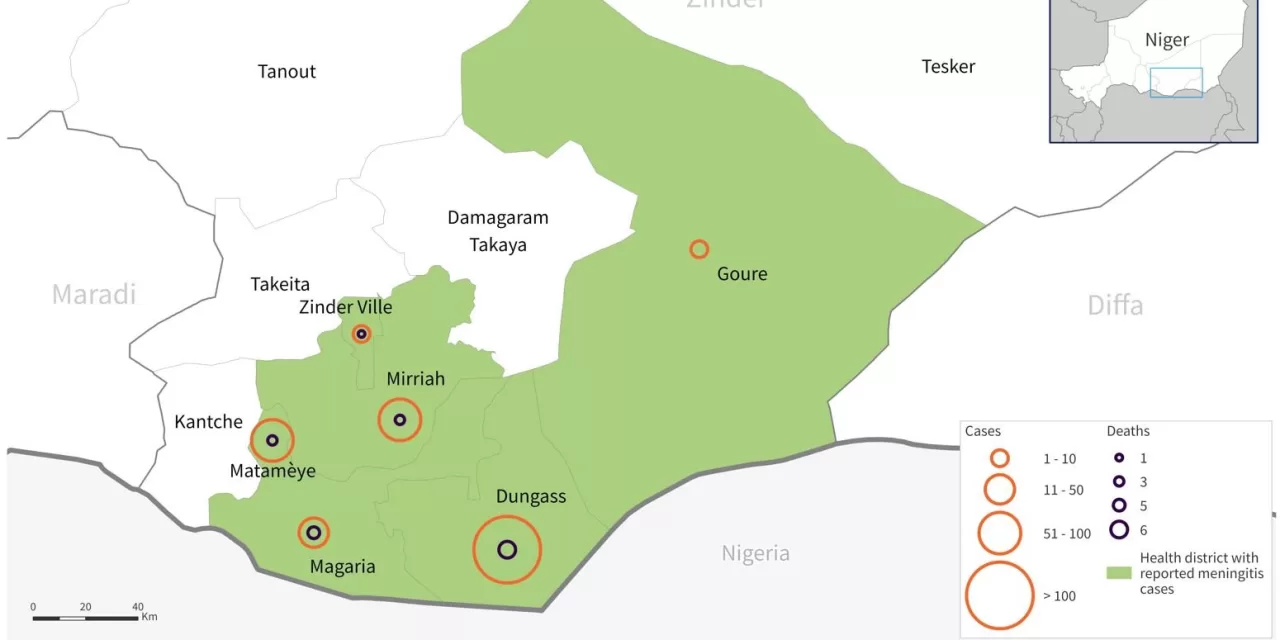
The most affected health district of Zinder region is Dungass (342 cases, 6 deaths), followed by Matamèye (98 cases, 3 deaths), Mirriah (72 cases, 3 deaths), Magaria (38 cases, 5 deaths), Zinder ville (7 cases, 1 death) and Gouré (2 cases, 0 deaths).
Figure 1. Distribution of reported meningitis cases by health district, Zinder region, Niger, 1 November 2022 – 27 January 2023. 
Epidemiology of meningitis
Meningitis is a serious infection of the meninges, the membranes covering the brain and spinal cord. Several different bacteria can cause meningitis, however, Streptococcus pneumoniae, Haemophilus influenzae, Neisseria meningitidis (N. meningitis) are the most frequent ones, and are transmitted from person to person through droplets of respiratory or throat secretions from infected people.
A total of 12 serogroups of N. meningitidis have been identified, six of which (A, B, C, W, X and Y) can cause meningococcal meningitis epidemics.
The average incubation period is 4 days but can range between 2 and 10 days. The most common symptoms of meningitis are a stiff neck, high fever, sensitivity to light, confusion, headaches and vomiting. Even with early diagnosis and adequate treatment, 5% to 10% of patients die, typically within 24 to 48 hours after the onset of symptoms. Bacterial meningitis may result in brain damage, hearing loss or a learning disability in 10% to 20% of survivors. A less common, but even more severe (and often fatal), form of meningococcal disease is meningococcal septicaemia, which is characterized by a haemorrhagic rash and rapid circulatory collapse.
The highest burden of disease is seen in a region of sub-Saharan Africa, known as the African Meningitis Belt, which is especially recognised to be at high risk of meningococcal but also pneumococcal meningitis epidemics.
Niger is located largely in the African meningitis belt, where meningitis epidemics typically follow a seasonal pattern (usually from January to June), with a size that varies from year to year. In 2015, a large meningitis outbreak attributed to NmC occurred, affecting nearly 10 000 people. In 2009 and 2006, meningitis outbreaks caused by N. meningitidis serogroups A (NmA) and X (NmX), respectively, were also reported. Haemophilus influenzae and Streptococcus pneumoniae are two other important pathogens that contribute significantly to the bacterial meningitis burden within Niger.
Licensed vaccines against meningococcal, pneumococcal and haemophilus influenzae diseases have been available for many years. These bacteria have several different strains (known as serotypes or serogroups) and vaccines are designed to protect against the most harmful strains. Over time, there have been major improvements in strain coverage and vaccine availability, but no universal vaccine against these infections exists.
In the African meningitis belt, meningococcus serogroup A accounted for 80–85% of meningitis epidemics before the introduction of a meningococcal A conjugate vaccine through mass preventive campaigns (since 2010) and into routine immunization programmes (since 2016). Among vaccinated populations, incidence of serogroup A meningitis has declined by more than 99%, and no serogroup A case has been confirmed since 2017.
However, cases of meningitis and outbreaks due to other meningococcal serogroups, apart from serogroup B, continue to strike.
Public health response
- A technical committee has been established in the Zinder region to coordinate the response to the epidemic. The meningitis response plan has been finalized and implemented. An international team from WHO and other partners including MSF and UNICEF has been deployed to support the response.
- Surveillance system activities have been reinforced in the Zinder region especially in Dungass health district, including case investigations. Laboratory activities are ongoing, including sample collection and confirmation from suspected meningitis cases.
- Case management activities have been strengthened, including procurement of the antibiotic ceftriaxone, cases isolation, deployment of health workers for case management, distribution of case management guidelines and provision of free treatment to cases.
- A request for 608 960 doses of trivalent ACW polysaccharide vaccine was approved and delivered by the International Coordinating Group (ICG) on Vaccine Provision in two batches of approximately 300 000 doses each on 31 December 2022 and 9 January 2023.
- Reactive vaccination campaigns with the trivalent ACW meningococcal polysaccharide vaccine have been implemented by the MoH with the support of WHO and The Global Alliance for Vaccines and Immunization (GAVI) in the Health Districts of Dungass, Gouré, Mirriah and Matamèye, targeting the age group 2 to 29 years. The overall vaccination coverage reached is 99.8%.
- Risks communication and community engagement activities are ongoing in close cooperation with administrators and community leaders in affected districts, delivering health advice and infection, prevention and control recommendations through community radios and other channels, including door-to-door sensitisation on the need to immediately seek medical assistance if symptoms occur to promptly start treatment.
WHO risk assessment
The ongoing outbreak shows both an increased number of cases and an increased growth rate compared to the previous seasons.
Moreover, the meningitis epidemic season (usually from January to June, marked by high temperatures and dry winds combined with heavy dust, a period known as the harmattan), the mixing of populations, the simultaneous occurrence of other epidemics in the same region (measles, diphtheria and COVID-19), insecurity and population displacement, all in the context of a protracted humanitarian crisis, are likely to contribute to the spread of the outbreak.
The Zinder region borders Jigawa State in Nigeria, where a NmC outbreak is also ongoing, confirming the risk of international spread to other countries of the West African subregion.
WHO assesses the risk posed by the current meningitis outbreak in Niger as high at the national level, moderate at the regional level, and low at the global level.
WHO advice
Meningococcal meningitis remains a public health concern with a high case fatality rate and leading to serious long-term complications.
Preventing meningitis through vaccination is the most effective way to reduce the burden and impact of the disease by delivering long-lasting protection. The rollout of multivalent meningococcal conjugate vaccines is a public health priority to eliminate bacterial meningitis epidemics in the African meningitis belt. Introduction into routine immunization programmes and maintaining high coverage will be critical to avoid the resurgence of epidemics.
Antibiotics for close contacts of meningococcal cases, when given promptly, decrease the risk of transmission. Outside the African meningitis belt, chemoprophylaxis is recommended for close contacts within the household. Within the meningitis belt, chemoprophylaxis for close contacts is recommended in non-epidemic situations. Ciprofloxacin is the antibiotic of choice, and ceftriaxone an alternative.
Admission to a hospital or health centre is necessary. Isolation of the patient is not usually advised after 24 hours of treatment.
Appropriate antibiotic treatment must be started as soon as possible. Ideally, lumbar puncture should be done first as antibiotics can make it more difficult to grow bacteria from the spinal fluid. However, blood sampling can also help to identify the cause and the priority is to start treatment without delay. A range of antibiotics is used to treat meningitis, including penicillin, ampicillin, and ceftriaxone. During epidemics of meningococcal and pneumococcal meningitis, ceftriaxone is the drug of choice.
The response to epidemics consists of appropriate case management, active community-based case-finding and reactive mass vaccination of affected populations. Surveillance, from case detection to investigation and laboratory confirmation is essential to the control of meningitis.
Reactive vaccination campaigns have been implemented in Zinder region, and monitoring the spread to new areas is crucial to guide further response activities, including considering further vaccine requests if appropriate. Timeliness of the reactive campaign is critical, ideally within four weeks of crossing the epidemic threshold.
WHO does not recommend any restriction on travel and trade to Niger on the basis of the information available on the current event.
Further information
- WHO. Health topics, Meningitis
- WHO. Meningitis fact sheets
- Defeating meningitis 2030: baseline situation analysis
- Defeating meningitis 2030: global roadmap
- WHO. Immunization, Vaccines and Biologicals. Meningococcal meningitis
- WHO AFRO. Meningococcal Meningitis.
- WHO AFRO: Outbreaks and Emergencies Bulletin
Citable reference: World Health Organization (8 February 2023). Disease Outbreak News; Meningitis – Niger. Available at https://www.who.int/emergencies/disease-outbreak-news/item/2023-DON439