On 8 June 2023, after two consecutive incubation periods (42 days) without a new confirmed case reported, the Ministry of Health of Equatorial Guinea declared the end of the Marburg virus disease (MVD) outbreak, as per the WHO recommendations. A total of 17 confirmed and 23 probable cases were reported from five districts in four provinces; 12 of the 17 confirmed cases died and all of the probable cases were reported deaths.
WHO and partners provided technical support to the government to contain this outbreak through its country office.
WHO encourages maintaining most response activities for three months after the outbreak ends. This is to make sure that if the disease re-emerges, health authorities are able to detect it immediately, prevent the disease from spreading again, and ultimately save lives.
Description of the situation
On 13 February 2023, the Ministry of Health and Social Welfare of Equatorial Guinea declared an outbreak of MVD after suspected viral hemorrhagic fever deaths were reported between 7 January and 7 February 2023, and a case tested positive on 12 February for Marburg virus by real-time polymerase chain reaction (RT-PCR) at the Institut Pasteur de Dakar in Senegal.
From the outbreak declaration until 7 June 2023, 17 confirmed and 23 probable cases were reported in the continental region of Equatorial Guinea. Twelve of the confirmed cases died and all of the probable cases were reported deaths (the case fatality ratio among confirmed cases is 75%, excluding one confirmed case with an unknown outcome).
The last confirmed case admitted to a Marburg treatment center in Bata district in Litoral province was discharged on 26 April, after two consecutive negative PCR tests for MVD. On 8 June 2023, after two consecutive incubation periods (42 days) without a new confirmed case reported, the Ministry of Health of Equatorial Guinea declared the end of the outbreak.
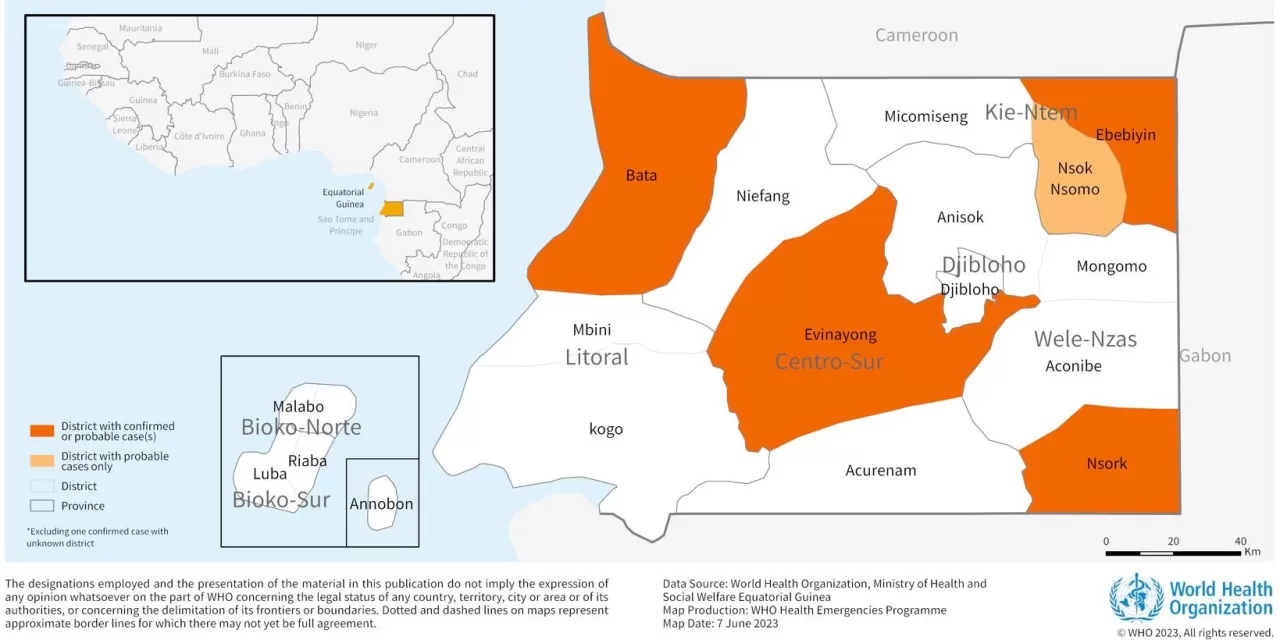
Confirmed or probable cases were reported in five districts (Bata, Ebebiyin, Evinayong, Nsok Nsomo and Nsork) in four of the country’s eight provinces (Centro Sur, Kié-Ntem, Litoral and Wele-Nzas).
Five cases (31%) were identified among healthcare workers, of whom two died (CFR among HCWs: 40%).
Four patients recovered and were enrolled in a survivor care programme to receive psychosocial and other post-recovery support.
Figure 1. MVD cases by week of symptoms onset* and case classification, Equatorial Guinea, as of 7 June 2023.
Figure 2. Map of districts reporting MVD confirmed and probable cases during the outbreak, Equatorial Guinea. 
Epidemiology of Marburg virus disease
Marburg virus spreads between people via direct contact through broken skin or mucous membranes with the blood, secretions, organs or other bodily fluids of infected people, and with surfaces and materials such as bedding, and clothing contaminated with these fluids. Healthcare workers have previously been infected while treating suspected or confirmed MVD patients. Burial ceremonies that involve direct contact with the body of the deceased can also contribute to the transmission of Marburg virus.
The incubation period varies from two to 21 days. Illness caused by Marburg virus begins abruptly, with high fever, severe headache, and severe malaise. Severe haemorrhagic manifestations may appear between five and seven days from symptom onset, although not all cases have haemorrhagic signs, and fatal cases usually have some form of bleeding, often from multiple areas.
Although no vaccines or antiviral treatments are approved to treat the virus, Remdesivir was used in this outbreak on compassionate care basis. Supportive care – rehydration with oral or intravenous fluids – and treatment of specific symptoms improve survival. A range of potential treatments are being evaluated, including blood products, immune therapies, and drug therapies.
This was the first documented outbreak of MVD reported in Equatorial Guinea. Another MVD outbreak was recently declared over in the United Republic of Tanzania (for more information, see the Disease Outbreak News published on 2 June 2023). MVD outbreaks have been previously reported in Ghana (2022), Guinea (2021), Uganda (2017, 2014, 2012, 2007), Angola (2004-2005), the Democratic Republic of the Congo (1998 and 2000), Kenya (1990, 1987, 1980) and South Africa (1975).
Public health response
Coordination
- Following the official outbreak declaration in the country, the Government of Equatorial Guinea established an emergency response structure to manage the response in the continental region with supporting partners and developed an initial three-month operational response plan.
- A transition and recovery plan for a one-year period has been developed. This plan will be implemented under leadership from the Ministry of Health, with support from partners, including WHO.
- Partners from the Global Outbreak Alert and Response Network (GOARN) were mobilized to assist in response activities. Several experts have been deployed through WHO to support case management, laboratory, epidemiology, and surveillance functions.
- WHO supported the Ministry of Health in providing training for surveillance activities, including case investigation, contact tracing, active case search in health facilities and the community, and in supervising field teams.
- The UN system, including WHO, continues to advocate for the Prevention of Sexual Exploitation and Abuse as it awaits government agreement to undertake community-based activities.
Partner Support
- Several partners supported the government-led response through the provision of technical, financial and operational support. These include WHO, the US Centers for Disease Control and Prevention (US-CDC), the Cuban Medical Brigade, the Africa Centre for Disease Control and Prevention (Africa CDC), the International Federation of the Red Cross and Red Crescent Societies (IFRC), and the United Nations Children’s Fund (UNICEF).
Surveillance
- WHO supported the establishment of the alert and dispatch center for MVD alert management.
- WHO provided training and supportive supervision of surveillance activities, including case investigation and contact tracing and coordinating with healthcare facilities for active surveillance.
Laboratory
- With the support of the US Centers for Disease Control and Prevention, and WHO, laboratories with RT-PCR capacities were set up initially in Ebebiyin and then in Bata.
- MVD diagnostic and sequencing capacities were subsequently implemented in Malabo at the Baney laboratory with support from Institut Pasteur Dakar and WHO, as well as other partners.
- WHO continues to support laboratory operations as well as specimen transportation notably through the training of shippers of infectious substances.
Clinical care
- WHO supported the MoH in the establishment of the Mondong Treatment Center in Bata and in the coordination of a referral system, including three ambulances that can retrieve suspected and confirmed patients from any district in the region and bring them to the Mondong treatment center.
- WHO also supported the MoH in the establishment of a survivor clinic that provides medical and psychological care and testing to survivors.
Infection Prevention and Control (IPC) and WASH (Water, Sanitation and Hygiene)
- WHO supported the establishment of the MoH regional IPC task force for coordination of IPC activities which met daily.
- In collaboration with MOH and US CDC, WHO supported the development and implementation of the National Strategy for the IPC response which was endorsed by MOH and implemented by key partners including UNICEF and Africa CDC.
- WHO developed IPC technical guidance and other products including Standard Operating Procedures, checklists, training materials and tools as needed.
- WHO supported the MoH in developing a rapid health care facility evaluation tool on IPC measures in place (such as screening and isolation capacity), including making this tool available online.
- WHO provided IPC training modules in the context of MVD, which were adopted and used to train health workers in all the affected districts as well as adopted by key implementing partners.
- WHO operational support and logistics (OSL) and UNICEF identified key IPC supplies required (including personal protective equipment, alcohol-based hand rub, etc).
- WHO worked with partners to advocate for improved Water, Sanitation and Hygiene in health facilities, in particular water supply and waste management.
- WHO supported the establishment, training and implementation of decontamination and safe and dignified burial teams.
- WHO recruited and trained five national IPC focal points in Bata, Ebibeyin, Mongomo, Evinayong and Malabo.
Risk Communication and Community Engagement (RCCE)
- WHO supported MoH in the development of an RCCE national plan and establish an RCCE coordination with key partners (UNICEF, IFRC, Africa CDC, among others) to ensure timely, relevant and actionable RCCE messaging, and activities reach affected and at-risk populations.
- Intensive and tailored public awareness, strategic networking, and capacity building for RCCE national experts, social mobilizers, and community leaders were implemented in all the affected districts.
- Religious leaders, decision-makers, school delegates, volunteers, media professionals, etc. were engaged to enhance community involvement in the response.
Border health and points of entry
- On 26 April 2023, WHO organized a webinar with the support of the US-CDC and the International Organization for Migration (IOM) to raise awareness on the necessary border health readiness and response activities in the context of MVD outbreaks for affected and neighboring countries.
Operational support and logistics (OSL)
- WHO has provided operational and logistics support and maintenance of the Marburg treatment centre, including structural rehabilitation, provision of electricity and water, and supply chain management.
- WHO established support for fleet management, including three ambulances on standby 24/7 at the Bata treatment centre, and approximately 20 vehicles.
- WHO has provided essential medicines and supplies to all pillars.
- WHO established a central warehouse for essential items in Bata, which supports distribution to other areas.
Readiness and preparedness in neighboring countries
- Readiness activities were scaled up in the neighbouring countries of Cameroon and Gabon to detect as early as possible any suspected case. All alerts from these neighbouring countries were investigated to rule out MVD.
- WHO developed a readiness checklist to assist neighbouring countries in assessing their level of readiness, and identifying potential gaps and concrete actions to be taken in case of any potential outbreak of filovirus including MVD. The checklist consists of several key components and an average score is calculated to provide readiness scores to each of the identified countries. A second round of readiness assessment across all pillars was conducted for Cameroon and Gabon.
- Based on the gaps identified during the assessments, a gap analysis was conducted and shared with Cameroon and Gabon to inform priority readiness activities. The identified gaps were addressed through the optimization of operational capacities and capabilities using various strategies, including trainings, table-top exercises, and simulation exercises. Additionally, experts were deployed to support the implementation of the readiness activities.
WHO risk assessment
In compliance with WHO recommendations, the criteria to declare the end of an outbreak after two maximum incubation periods (42 days) was observed with no new confirmed or probable case of MVD detected.
Based on knowledge of past outbreaks of filovirus disease, there remains a risk of re-emergence of MVD even following the declaration of the end of the outbreak. Undetected transmission of Marburg virus may exist in the country; not all chains of transmission were definitively linked, and one confirmed case was never identified. The initial source of the outbreak has not been identified, and a new emergence of disease is possible, including from interaction with animal reservoirs. The virus may also persist for an extended period in body fluids of survivors, including semen, underlying the importance of their participation in the survivors program, and the support the program provides.
Based on the available information at the end of MVD outbreak in Equatorial Guinea, the risk of MVD remerging is considered as low at the national level, low at the subregional level, regional level and at the global level.
WHO advice
The current WHO recommendation is that most response activities continue for three months after the outbreak ends, to make sure that if the disease re-emerges, health authorities can detect it right away, prevent the disease from spreading, and ultimately save lives.
WHO advises the following risk reduction measures as an effective way to reduce MVD transmission:
- Reducing the risk of bat-to-human transmission arising from prolonged exposure to mines or caves inhabited by fruit bat colonies. During work or research activities or tourist visits in mines or caves inhabited by fruit bat colonies, people should wear gloves and other appropriate protective clothing (including masks). During outbreaks, all animal products (blood and meat) should be thoroughly cooked before consumption.
- Health facilities should ensure IPC measure programs are in place including screening for cases of MVD, training of health workers on IPC practices, safe injection practices, environmental cleaning and disinfection protocols are in place, decontamination of reusable medical devices and safe waste management.
- Health workers caring for patients with confirmed or suspected MVD should apply transmission-based precautions in addition to standard precautions, including appropriate use of personal protective equipment and hand hygiene according to the WHO 5 moments to avoid contact with patients’ blood and other body fluids and with contaminated surfaces and objects.
- Surveillance activities should be strengthened to ensure early detection of any future cases.
- Raising community awareness of the risk factors for Marburg virus infection and the protective measures individuals can take to reduce human exposure to the virus is key to reducing human infections and deaths. This includes reminders for persons with symptoms to immediately seek care in health facilities to reduce the risk of transmission in the community and to receive treatment, thereby improving chances for recovery. Community and family members should avoid caring for symptomatic individuals at home, avoid touching bodies of people deceased with MVD symptoms, other potentially contaminated items, and surfaces, and encourage them to go to a health facility for assessment and treatment.
WHO advises against applying international travel and/or trade measures to Equatorial Guinea.
Further information
- República de Guinea Ecuatorial. Ministerio de Sanidad y Bienestar Social. Actualización de datos epidemiológicos
- WHO Marburg Virus Disease outbreak in Equatorial Guinea ends
- WHO Marburg virus disease outbreak in Equatorial Guinea
- World Health Organization (8 May 2023). Disease Outbreak News; Marburg virus disease – Equatorial Guinea and the United Republic of Tanzania. Available at https://www.who.int/emergencies/disease-outbreak-news/item/2023-DON467
- World Health Organization (15 April 2023). Disease Outbreak News; Marburg virus disease – Equatorial Guinea. Available at https://www.who.int/emergencies/disease-outbreak-news/item/2023-DON459
- World Health Organization (22 March 2023). Disease Outbreak News; Marburg virus disease – Equatorial Guinea. Available at https://www.who.int/emergencies/disease-outbreak-news/item/2023-DON449
- World Health Organization (25 February 2023). Disease Outbreak News; Marburg virus disease – Equatorial Guinea. Available at https://www.who.int/emergencies/disease-outbreak-news/item/2023-DON444
- WHO Equatorial Guinea confirms first-ever Marburg virus disease outbreak
- WHO Urgent Marburg Meeting
- WHO Ebola and Marburg virus disease epidemics: preparedness, alert, control, and evaluation
- WHO Infection Prevention and Control guidance for care of patients with suspected or confirmed Filovirus haemorrhagic fever in health-care settings, with focus on Ebola
- WHO Water and sanitation for health facility improvement tool (WASH FIT)
- World Health Organization. (2016). Personal protective equipment for use in a filovirus disease outbreak: rapid advice guideline. World Health Organization. https://apps.who.int/iris/handle/10665/251426
- WHO recommended criteria for declaring the end of the Ebola virus disease outbreak
- WHO Ebola Virus Disease (EVD): Key questions and answers concerning health-care waste
- WHO Factsheet – Marburg virus disease
- WHO Questions and Answers – Marburg virus disease
- Organisation mondiale de la Santé. (2014). Flambées épidémiques de maladie à virus Ebola et Marburg : préparation, alerte, lutte et évaluation. Organisation mondiale de la Santé. https://apps.who.int/iris/handle/10665/130161
- WHO. Introduction to Marburg Virus Disease
Citable reference: World Health Organization (9 June 2023). Disease Outbreak News; Marburg virus disease – Equatorial Guinea. Available at https://www.who.int/emergencies/disease-outbreak-news/item/2023-DON472