Following the launch of the national trachoma control programme by the Ministry of Health in 2011, the National Trachoma Task Force team stipulated the need for integration of the programme within the Ministry of Health structure. Malawi received its first azithromycin (Zithromax®, Pfizer, New York) donation from the International Trachoma Initiative in 2011 to conduct antibiotic mass drug administration. Following the development of its Trachoma Action Plan in 2012–2013 and its rollout in 2014, funding to implement the SAFE strategy in all endemic districts was made possible through financial support from the Queen Elizabeth Diamond Jubilee Trust in 2014. Medium cadre ophthalmic clinicians were trained and certified as trachomatous trichiasis (TT) surgeons. A quality assurance team was formed, and regular national trachoma coordination meetings were conducted. The Ministry of Health also undertook awareness raising campaigns about the importance of facial cleanliness and personal hygiene in the fight against trachoma. Furthermore, stakeholders already present in the districts intensified their work and implementing water, sanitation and hygiene activities resulted in significant improvements in the availability of safe water and access to improved sanitation.
Malawi and WHO will continue to closely monitor previously endemic populations to ensure there is a rapid, proportionate response to any resurgence of disease.
Globally, Malawi joins 14 other countries that have been validated by WHO for having eliminated trachoma as a public health problem. These are Cambodia, China, the Islamic Republic of Iran, the Lao People’s Democratic Republic, the Gambia, Ghana, Mexico, Morocco, Myanmar, Nepal, Oman, Saudi Arabia, Togo and Vanuatu.
Disease prevalence
Trachoma remains a public health problem in 42 countries with an estimated 125 million people living in areas endemic for the disease. Trachoma is found mainly in the poorest and most rural areas of Africa, Central and South America, Asia, the Western Pacific and the Middle East. The African Region is disproportionately affected by trachoma with 105 million people living in at-risk areas, representing 84% of the global trachoma burden.
Significant progress has been made over the past few years and the number of people requiring antibiotic treatment for trachoma in the African Region fell by 84 million from 189 million in 2014 to 105 million as of June 2022.
Following Malawi’s success, trachoma remains endemic in 25 countries2 in WHO’s African Region, bringing us closer towards the elimination target for trachoma set out in the NTD road map 2021–2030.
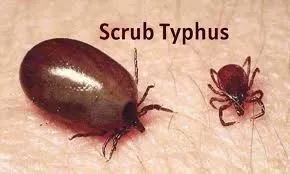
The disease
Trachoma is the leading infectious cause of blindness and is caused by infection with the bacterium Chlamydia trachomatis. Infection spreads from person to person through contaminated fingers, fomites, and flies that have come into contact with discharge from the eyes or nose of an infected person. Environmental risk factors for trachoma transmission include poor hygiene, overcrowded households, inadequate access to water and inadequate access or use of proper sanitation facilities.
Trachoma is an endemic disease that mostly burdens underserved remote rural communities. Infection mainly affects children, becoming less common with increasing age. Repeated infections in early childhood result in late complications years and even decades later. In adults, women are twice as likely than men to be affected by the blinding complications of trachoma, mainly due to their close contact with infected children.
Repeated infections in childhood lead to scarring of the inner side of the upper eyelids. In some individuals this leads to trachomatous trichiasis (TT), where one or more eyelashes on the upper eyelids touch the eye. TT is a debilitating condition resulting in extreme pain with each blinking action of the eyelids. TT can be managed surgically, but, if left untreated, may lead to scarring of the cornea, resulting in visual impairment and blindness. Trachoma can be eliminated using WHO’s SAFE strategy.3
GET2020
In 1996, WHO launched the WHO Alliance for the Global Elimination of Trachoma by the year 2020 (GET2020). With other partners in the Alliance, WHO supports country implementation of the SAFE strategy and strengthening of national capacity through epidemiological assessment, monitoring, surveillance, project evaluation and resource mobilisation contributing towards the elimination of trachoma as a public health problem. The NTD road map 2021–2030, endorsed by the World Health Assembly in 2020 through decision 73(33), sets 2030 as the new target date for global elimination.
1. Elimination of trachoma as a public health problem is defined as: (i) a prevalence of trachomatous trichiasis “unknown to the health system” of <0.2% in adults aged ≥15 years (approximately 1 case per 1000 total population), and (ii) a prevalence of trachomatous inflammation—follicular in children aged 1–9 years of <5%, sustained for at least two years in the absence of ongoing antibiotic mass treatment, in each formerly endemic district; plus (iii) the existence of a system able to identify and manage incident trachomatous trichiasis cases, using defined strategies, with evidence of appropriate financial resources to implement those strategies.
2. Algeria, Angola, Benin, Burkina Faso, Cameroon, Central Africa Republic, Chad, Cote d’Ivoire, Democratic Republic of the Congo, Eritrea, Ethiopia, Guinea, Guinea-Bissau, Kenya, Mali, Mauritania, Mozambique, Niger, Nigeria, Senegal, South Sudan, United Republic of Tanzania, Uganda, Zambia and Zimbabwe.
3. The SAFE strategy consists of Surgery to treat the late complication (trachomatous trichiasis); Antibiotics to clear infection, particularly mass drug administration of the antibiotic azithromycin, which is donated by the manufacturer, Pfizer, to elimination programmes through the International Trachoma Initiative; and Facial cleanliness and Environmental improvement, particularly improved access to water and sanitation, to reduce transmission.