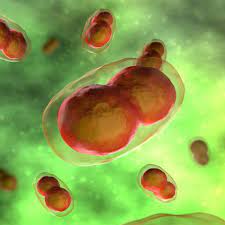
A recent study by researchers at the University of California, San Francisco (UCSF) has found that long-acting injectable antiretroviral therapy (LA-ART) can effectively manage HIV in patients who face challenges adhering to daily oral medication regimens. This approach not only aids in viral suppression but also holds potential in curbing the transmission of HIV.
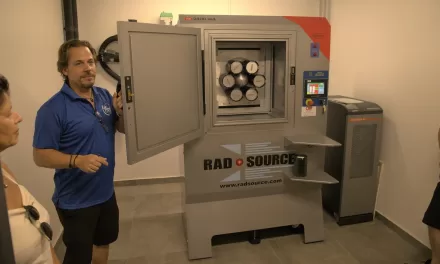
In 2021, federal regulators approved the first LA-ART injectable, combining cabotegravir and rilpivirine, for HIV patients who had previously achieved viral suppression with oral medications. However, the UCSF study aimed to evaluate its efficacy in patients who had not maintained viral control with pills, including those with housing instability, substance use disorders, or difficulties with pill swallowing or adherence.
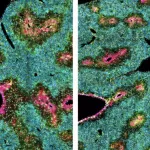
Participants received monthly or bimonthly injections, and their viral loads were monitored over 48 weeks. The results were promising, with over 98% of participants in both groups achieving “viral suppression,” defined as undetectable levels of HIV. This study stands as the largest and longest comparison of its kind, highlighting the potential of injectable therapies for diverse patient populations.
Dr. Matthew Spinelli, assistant professor in the Division of HIV, Infectious Diseases, and Global Medicine at UCSF, remarked, “These long-acting treatments are likely to be transformative for people in this population.” He added that some patients who struggled for years with daily pills experienced significant improvements after switching to injectable therapy, describing the change as “like magic.”
By offering an alternative to daily oral medications, LA-ART provides hope for individuals who face barriers to adherence, potentially improving health outcomes and reducing the risk of HIV transmission.
Disclaimer: This article is based on information from the UCSF study as reported by Medical Xpress. For comprehensive details, please refer to the original source.