Dr Pedro Alonso, Director, WHO Global Malaria Programme
/news/boy-on-bicycle-drc.png?Status=Master&sfvrsn=5f98425e_5)
Dear friends and partners,
After more than 7 years with WHO, I will be retiring today from my position as Director of the WHO Global Malaria Programme (GMP). It has been a great pleasure and honor to work with so many committed and inspiring colleagues, malaria programme staff and partners around the world. Together, we have accomplished many things in our journey towards a malaria-free world!
As I reflect on my years with WHO, I am immensely proud of our collective work in the areas that you will find outlined below. Many of you reading this message have contributed to these projects and initiatives, and your support is greatly appreciated.
- Responding to the double challenge of malaria and COVID-19
- Catalyzing the “High burden high impact initiative” (HBHI)
- Supporting countries with a low malaria burden through the “E-2020 initiative”
- Certifying 9 more countries as malaria-free since 2015
- Clarifying WHO’s position on the malaria eradication
- Delivering a WHO recommendation on RTS,S, the first malaria vaccine
- Tackling biological threats to malaria control
- Stepping up malaria responses in complex emergency settings
- Reforming WHO’s processes for developing and disseminating malaria guidance
- Updating the WHO global malaria strategy
At the same time, I take no satisfaction in where we stand today, and I leave in many ways with a heavy heart. How can I be satisfied when we continue to report more than 200 million new cases of malaria annually, and more than 600 000 malaria-related deaths? There is simply no room for satisfaction or content.
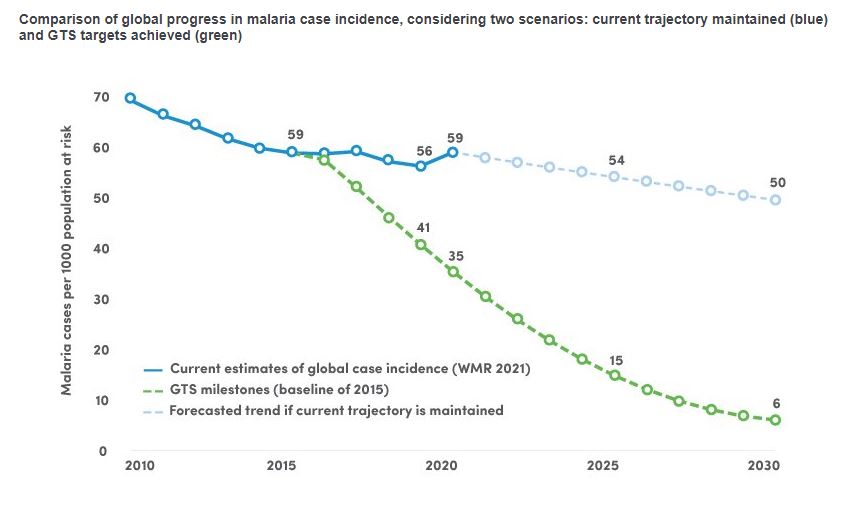
As we are all aware, progress towards 2 strategic 2020 milestones of the global strategy were missed. In 2020, the global malaria case incidence rate was 59 cases per 1000 people at risk, against a target of 35 – off track by 40%. The global mortality rate was 15.3 deaths per 100 000 people at risk, against a target of 8.9 – off track by 42%.
Comparison of global progress in malaria case incidence, considering two scenarios: current trajectory maintained (blue) and GTS targets achieved (green)
/word-malaria-report/gts-worldwide-nl.jpg?Status=Master&sfvrsn=1db9579a_8)
Since 2015, 24 countries have registered increases in their malaria mortality rate, and a further 14 countries, all of them in the WHO African Region, have remained at similar levels of malaria mortality. Although an estimated 1.7 billion malaria cases and 10.6 million deaths were averted between 2000 and 2020, the hard truth is that we have approximately the same number of cases today as we did 20 years ago.
The trends seen in sub-Saharan Africa are especially worrying: malaria cases and deaths remain unacceptably high, and a convergence of biological threats poses an added challenge for disease control efforts. Furthermore, a number of malaria-endemic countries in the region have faced devastating humanitarian emergencies over the last 2 years, beyond COVID-19 – from Ebola outbreaks to conflicts and flooding. While it is difficult to quantify the impact of these emergencies, they have clearly caused disruptions in access to malaria services.
Taken together, we are facing a malaria crisis.
We need to do things differently. As Einstein famously said, doing the same thing over and over again and expecting a different result is insanity. We need to adopt a new, problem-solving mindset in which malaria control is not simply seen as a managerial task to be performed, but as a public health problem that challenges us all.
Too many people still miss out on the malaria interventions they need. Poor, marginalized populations are particularly vulnerable as they are more likely to become sick, less able to access quality services and hardest hit when they become ill. Ensuring a more equitable access to prevention and treatment tools for the most vulnerable must be a central strategy in our efforts to tackle this disease.
We have lived through a golden era. New tools and unprecedented financial resources delivered stunning achievements in the first 15 years of this century, representing one of the best success stories in global health. However, these gains are fragile, and we have seen the limits of what can be achieved with currently available tools and resources. I hope that the current malaria crisis catalyzes fresh momentum in the fight against this disease, unequivocally led by the affected countries themselves.
Thank you once again for your collaboration, commitment and friendship.
Pedro
Responding to the double challenge of malaria and COVID-19
In March 2020, before COVID-19 had secured a strong footing in Africa, WHO established a cross-partner mechanism to support malaria-endemic countries and ensure a coordinated response. Through weekly calls convened by the Global Malaria Programme, experts and leaders from more than 30 partner organizations shared updates on a variety of issues – from disruptions in the supply of key malaria commodities to the latest developments in clinical drug trials.
Through this collaborative work, we rapidly developed technical guidance to support countries in decisions around how to safely maintain malaria services in the context of the pandemic. Together with partners, we modelled the potential impact of health service disruptions on the malaria burden in sub-Saharan Africa; the resulting analysis, published in April 2020, reinforced our urgent call to countries to ensure the continuity of services that prevent, detect and treat the disease.
Heeding the call, malaria-endemic countries mounted impressive responses to the pandemic, adapting the way they deliver malaria services to the COVID-19 restrictions imposed by governments. Despite the inevitable disruptions to health services, countries and their development partners succeeded in averting the worst-case scenario projected by WHO. Nonetheless, we estimate that there were 69 000 more deaths and 14 million more cases in 2020 compared to 2019.
Catalyzing the “High burden high impact initiative” (HBHI)
In 2017, WHO sounded the alarm in its annual World malaria report on a plateau in progress and funding; all available data were pointing in this direction. Furthermore, out estimates showed that a small number of countries carried a large share of the global malaria burden and, in many of these countries, malaria was on the rise. Clearly, a “business as usual” approach to malaria control was not taking us where we needed to go.
Trends in malaria cases in 11 high burden countries, 2000–2020
/word-malaria-report/hbhi-trends-malaria-cases.png?Status=Master&sfvrsn=2602c35c_11)
The launch of “ High burden high impact” (HBHI), spearheaded by WHO and the RBM Partnership in 2018, marked a strategic shift in our efforts to tackle the disease. Over the last 3 years, the 11 participating HBHI countries – which, together, account for about 70% of the global malaria burden – are moving away from a “one-size-fits-all” approach to malaria control. Instead of applying the same mix of tools everywhere, they are selecting tailored packages of interventions based on local data and the local disease setting. I’m proud of the role that WHO played in developing this new conceptual model and supporting its implementation.
WHO’s support for the “Rethinking malaria” consultation, convened by Harvard University, is a parallel effort that goes beyond HBHI to consider the broader malaria venture that will needed to accelerate progress. It recognizes that the systems and structures that yielded success for the malaria community in the past will need to evolve to meet the challenges that lie ahead. The “Rethinking malaria” process drew heavily on the rich experiences from malaria-endemic countries, including those pioneering the HBHI approach.
The journey does not stop at the production of a report. The thinking now needs to be translated into the urgent action that is needed to get back on track. WHO in Africa is taking the lead on galvanizing the continent to identify how to make change happen and collectively secure equitable and sustainable solutions.
Supporting countries with a low malaria burden through the “E-2020 initiative”
Although progress has slowed or stalled in countries hardest hit by malaria, many countries with a low burden of the disease are moving steadily towards the goal of elimination. According to WHO’s latest World malaria report, more than half of malaria-endemic countries (47) had fewer than 10 000 cases per year in 2020 compared to 26 countries in the year 2020.
In 2017, WHO launched a targeted initiative, the “E-2020,” to support malaria-eliminating countries in their efforts to stamp out the disease. Over a 3-year period, “E-2020” member countries benefited from technical guidance and specialized support as they worked to eliminate the last vestiges of the disease.
/news/zeroing-on-malaria-elimination.png?Status=Master&sfvrsn=30422816_6) To keep elimination high on the agenda, WHO convened 3 global forums that brought together malaria programme managers from “E-2020” countries. The forums provided an important platform for technical experts from all regions to share progress, setbacks and lessons learned.
To keep elimination high on the agenda, WHO convened 3 global forums that brought together malaria programme managers from “E-2020” countries. The forums provided an important platform for technical experts from all regions to share progress, setbacks and lessons learned.
To support countries in their elimination journeys, we also created 2 advisory bodies. The Malaria Elimination Oversight Committee guides countries in their efforts to reach zero indigenous malaria cases, and the Malaria Elimination Certification Panel is tasked with verifying a country’s malaria-free status after reviewing available evidence, analyzing independent sources and conducting on-site evaluation missions.
By the end of 2020, 10 countries had reached the elimination milestone of WHO’s global malaria strategy by reducing their indigenous malaria cases to zero – a remarkable achievement in view of the COVID-19 pandemic. Building on the foundation of the “E-2020”, WHO launched a new initiative in April 2021 aimed at halting transmission of malaria in 25 more countries by the year 2025.
Certifying 9 more countries as malaria-free since 2015
Soon after I joined the Global Malaria Programme, Sri Lanka was certified by WHO as malaria-free – an achievement that inspired countries and made news headlines around the world. Since then, 8 other countries have been awarded a malaria-free certification including, most recently, China and El Salvador.
/photostory/2019-china-elimination/china-malaria-photo-essay-2019-3.jpg?Status=Master&sfvrsn=c64a022c_4)
WHO/C. McNab
China’s success in getting to zero is an impressive feat in view of the malaria burden it once carried: in the 1940s, the country reported an estimated 30 million cases of the disease annually – more cases than the Democratic Republic of the Congo, the country with the world’s second highest malaria burden, carries today.
Against the odds, El Salvador, a country with a dense population that is fully surrounded by malaria-endemic nations, also succeeded in stamping out indigenous transmission of the disease. El Salvador is the first country in Central America to be certified malaria-free by WHO and, globally, 40 countries or territories have reached this milestone. Together, they have shown the world that getting to zero is a viable goal for all countries, no matter how far off the target may seem today.
Clarifying WHO’s position on the malaria eradication
In 2015, we celebrated the remarkable gains that had been made against malaria in the first 15 years of this century. The malaria-focused target of the Millennium Development Goals, which called for halting and beginning to reverse the incidence of malaria, was met convincingly, and many partners had set their sights on the launch of an eradication effort.
In 2016, WHO established a Strategic Advisory Group on malaria eradication (SAGme) to analyse future scenarios for malaria, including eradication. As a first step our advisory group, comprised of leading scientists and public health experts, developed a report clarifying current terminology and affirming WHO’s longstanding commitment to the goal of eradication. Notably, SAGme members were unable to specify a realistic target date for eradication, nor calculate what such an effort would cost.
After a 3-year study of trends and future projections, members of this advisory body released a more detailed report of its findings and recommendations. While unequivocally supporting the goal of eradication, the 13-member group recognized that, with currently available tools, attaining that goal was still far from reach.
I remain a firm believer that the ultimate goal can only be eradication, consistent with a World Health Assembly resolution of 1955 and reaffirmed thereafter, including in a resolution adopted by the Assembly in May 2021. But we are fighting a very complex parasite and have lacked, so far, the transformative tools that will be needed to wipe out malaria in the world’s highest burden areas. As the SAGme rightly noted, one of the highest priorities for achieving a malaria-free world is a renewed R&D agenda that improves the knowledge base and products necessary for achieving eradication.
On this year’s World Malaria Day, WHO will shine a spotlight on the vital role of innovation in the fight against malaria – including the need for innovation both in new tools and in the way that currently available tools are delivered.
Delivering a WHO recommendation on RTS,S, the first malaria vaccine
RTS,S is a shining example of innovation at work and a scientific breakthrough. It is the first vaccine recommended by WHO not only for malaria, but also for a human parasitic disease of any kind. WHO’s historic recommendation in October 2021 was based on a review of the full package of evidence on RTS,S, including results from the WHO-coordinated Malaria Vaccine Implementation Programme (MVIP), the largest implementation study that WHO has undertaken in its 70-year history.
/photostory/malaria-vaccine-one-year-on/malaria-vaccine-first-babies-7.jpg?Status=Master&sfvrsn=b50a6434_4)
WHO/N. Thomas
To date, more than 900 000 children have been reached with at least one dose of RTS,S in Ghana, Kenya and Malawi. Three years on, data from the MVIP have shown that the vaccine is safe, feasible to deliver and reduces deadly severe malaria. If deployed widely, RTS,S will save tens of thousands of young lives – but only if it’s given a chance to work. Over the last year, we have witnessed the rapid scale-up of safe, effective COVID-19 vaccines in many parts of the world. Children at risk of malaria deserve that same level of attention and urgency.
RTS,S is an important first-generation vaccine that could be complemented in the future by other malaria vaccines with similar or higher efficacy. We hope that this scientific achievement will encourage others to join malaria vaccine field – with the ultimate goal of preventing illness and saving as many lives as possible.
Tackling biological threats to malaria control
In recent years, WHO colleagues and partners have been responding to a number of pressing biological threats, including parasite resistance to antimalarial drugs; the spread of falciparum parasite mutations that are undermining the effectiveness of rapid diagnostic tests; an invasive malaria vector that thrives in urban and rural areas; and mosquito resistance to the insecticides used in key vector control tools. The latest data on these 4 biological threats can be found in the WHO Malaria Threats Map.
WHO is particularly concerned about reports of emerging drug-resistant malaria in Africa. In collaboration with our colleagues in the African Region, the Organization is developing a strategy to tackle this threat which you will hear more about in the coming months.
Our experience in tackling antimalarial drug resistance in the Greater Mekong subregion has shown that success is possible. When I first joined WHO, Cambodia was an epicenter of drug-resistant malaria, threatening future gains against the disease across the subregion, and worldwide. In my first visit to Cambodia as GMP Director, the country was reporting about 4000 new malaria cases, on average, every month.
/news/mother-and-child-cambodia.png?Status=Master&sfvrsn=2ba973c4_8)
WHO/V. Sokhin
Several weeks ago, I returned to Cambodia in what was my last visit official visit with WHO, and I was amazed by how dramatically the situation had changed. With just 10 to 15 new malaria cases every month, Cambodia has become a prime example of what can be achieved through a well-executed and adequately resourced national malaria strategy. The country has launched a process to verify subnational areas as malaria-free and aims to fully interrupt malaria transmission nationwide within the next 24 months.
With support from WHO and partners, the Greater Mekong subregion, as a whole, has achieved a dramatic reduction in its malaria burden, from a peak of approximately 650 000 cases in 2012 to 82 000 cases in 2020. Notably, there has been a substantial decline in cases of P. falciparum malaria – a primary target in view of the ongoing threat posed by parasite resistance to antimalarial drugs.
Fears around the spread of antimalarial drug resistance to other regions have not materialized; while drug-resistant parasites continue to circulate in the subregion, they have not spread beyond the Greater Mekong. When first-line antimalarial treatments fail, alternative and efficacious drug regimens remain available. The so-called and much publicized “superbug” (partially resistant to artemisinin and resistant to piperaquine) is on the verge of disappearing. With available drugs, and through the deployment of smart, data-driven public health strategies, countries of the Greater Mekong are zeroing in on the goal of elimination.
Stepping up malaria responses in complex emergency settings
In 2015, I travelled on a WHO mission to Sierra Leone, when the country was in the throes of responding to the Ebola epidemic. I was struck, at the time, by how a major disease like malaria can fall into a blind spot in the context of a humanitarian crisis. Indeed, across Sierra Leone, malaria (and not Ebola) took the greatest toll that year on children and families.
Together with the Ministry of Health and partners, WHO launched a successful mass drug administration (MDA) campaign – a strategy that succeeded in rapidly reducing malaria cases in the capital city of Freetown. This, in turn, kept more people out of health facilities and reduced their risk of acquiring an Ebola infection. Through MDA, all individuals in a target population are given antimalarial medicines, often at repeated intervals, regardless of whether or not they show symptoms of the disease.
/news/smc-child-nigeria.png?Status=Master&sfvrsn=89f9432a_8)
WHO/P. Utomi Ekpei
A similar strategy was later deployed in north-eastern Nigeria in one of the largest humanitarian crises seen in recent years. In 2017, following an 8-year conflict, two thirds of health facilities had been completely or partially destroyed leaving millions of internally displaced persons at risk of malaria and other life-threatening diseases. In Borno State, the number of malaria cases and deaths soared, particularly among young children – reaching levels rarely seen before. The WHO strategy of age-targeted MDA, delivered in collaboration with the WHO polio teams, succeeded in significantly reducing cases and deaths among young children.
Reforming WHO’s processes for developing and disseminating malaria guidance
In 2018, WHO undertook an extensive review of our processes for developing and sharing guidance on malaria, with inputs sought from colleagues and partners across the globe. Three “pain points” were identified through this exercise: perceived lengthy processes; inconsistent recommendations; and the sub-optimal use of WHO’s malaria guidance at the country level.
Over the last few years, the Global Malaria Programme has taken steps to tackle these points head-on. All proposals for new or updated WHO recommendations are now channeled rapidly through guideline development groups (GDGs). In the last year alone, members of 4 GDGs convened by WHO gathered virtually to consider recommendations on vector control, chemoprevention, treatment and elimination. By the end of April 2022, WHO expects to issue new or revised recommendations on vector control, chemoprevention and elimination, with other updates planned later in the year across a number of technical areas.
We have also taken important steps to improve the way our guidance is packaged and shared, with a view to optimizing its uptake at the country level. In February 2021, WHO launched the consolidated WHO Guidelines for malaria, bringing together – for the first time – all of the Organization’s guidance on malaria in one web-based platform. All WHO malaria recommendations can also be found in an easy-to-navigate mobile app.
As you have probably heard me say before, WHO global guidance and policy recommendations are not intended to be prescriptive or to explain what should be done in every situation. They suggest “what to do”. It is then up to countries to define, according to local contextual factors, whether the guidance is useful and relevant to them. Implementation manuals from WHO provide advice on “how to” implement the guidance. For maximum impact, countries are encouraged to select tailored packages of interventions that are informed by local data and disease settings.
Updating the WHO global malaria strategy
While the revised global technical strategy retains the goals and milestones endorsed by the World Health Assembly in 2015, it considers lessons learned since 2015, including the stalling of progress and the impact of the COVID-19 pandemic. The strategy’s 5 guiding principles were reordered to place a greater emphasis on the critical role of country ownership, and a sixth principle was added to reflect that successful malaria responses are underpinned by resilient health systems. Other guiding principles focus on the need for strong surveillance systems, equity in access to health services, innovation in tools and approaches, and interventions that are tailored to local conditions. A new resolution adopted by the Assembly in May 2021 urged Member States to step up the pace of progress against malaria through plans and approaches that are consistent with WHO’s updated strategy.

/news/sagme-cover.png?Status=Master&sfvrsn=aa1ec274_7)









