Baltimore, MD – In a promising development for tackling multidrug-resistant (MDR) tuberculous meningitis, researchers at Johns Hopkins Children’s Center have identified four new antibiotic regimens that show potential in treating this severe form of tuberculosis (TB). The study, published on August 14 in Nature Communications, marks a significant advancement in the fight against a disease considered one of the deadliest forms of TB globally.
The preliminary research, which included testing on humans, rabbits, and mice, focuses on regimens composed primarily of antibiotics already approved by the U.S. Food and Drug Administration (FDA) or those under clinical trials. Despite TB meningitis being rare in the United States, it remains a major global health challenge, with the highest incidence in Southeast Asia and Africa.
Current FDA-approved treatments for TB do not specifically address TB meningitis, although drugs used for pulmonary TB are available. A previous study by Johns Hopkins, led by Dr. Sanjay Jain, found that the existing regimen for drug-resistant pulmonary TB—bedaquiline, pretomanid, and linezolid (BPaL)—is ineffective against TB meningitis due to limitations in crossing the blood-brain barrier.
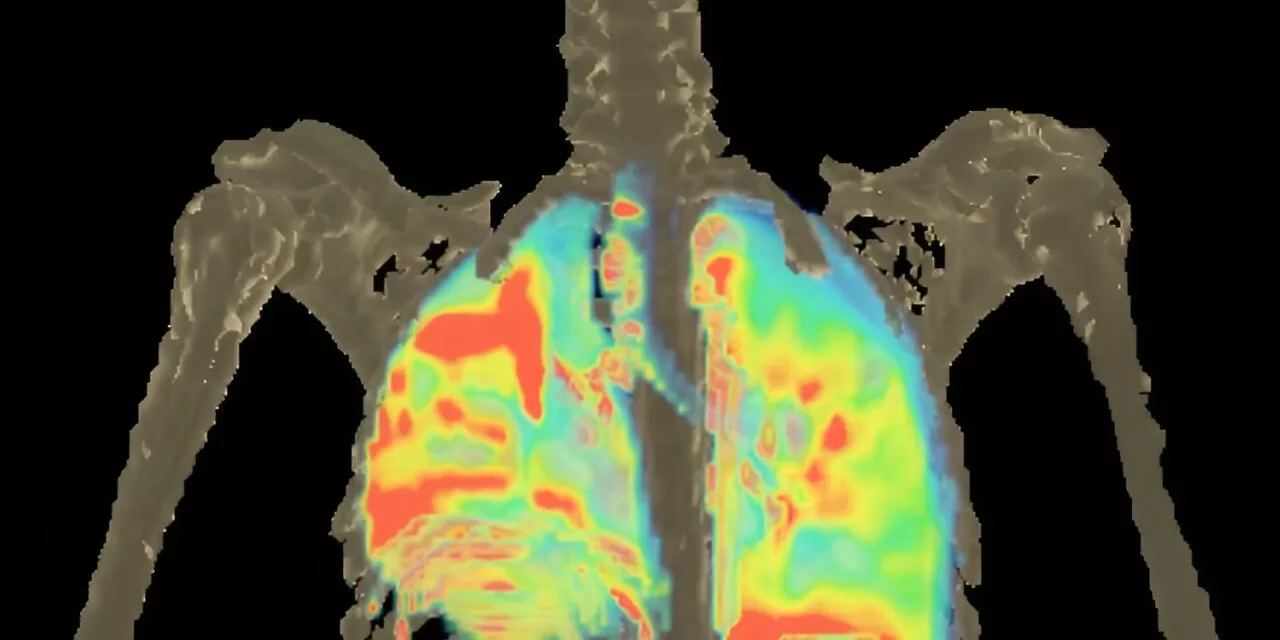
The new study utilized advanced imaging techniques, including positron emission tomography (PET) and computed tomography (CT), to evaluate how various antibiotics penetrate the brain and other tissues. Researchers created a modified, scan-friendly version of the antibiotic pretomanid to facilitate these assessments. The findings revealed that pretomanid penetrates the brain more effectively than the lungs, highlighting its potential for treating TB meningitis.
Dr. Xueyi Chen, a lead author of the study, emphasized the importance of distinguishing cerebrospinal fluid (CSF) levels of antibiotics from those in the brain, as CSF levels do not always correlate with brain levels. This discrepancy is crucial for understanding the effectiveness of treatments.
The researchers tested four antibiotics—pretomanid, sutezolid, linezolid, and bedaquiline—using animal models. Results showed that pretomanid achieved higher brain concentrations compared to the other antibiotics, which were more effective in lung tissues. Mathematical simulations further predicted that pretomanid is the most suitable for achieving therapeutic brain penetration.
The study identified three effective pretomanid-based regimens: BPa50LZ (bedaquiline, pretomanid, linezolid, pyrazinamide), Pa100LZ (pretomanid, linezolid, pyrazinamide), and Pa50LMxZ (pretomanid, linezolid, moxifloxacin, pyrazinamide). Each showed superior efficacy in treating TB meningitis compared to standard regimens. Additionally, a fourth regimen, Pa100SMx (pretomanid, sutezolid, moxifloxacin), proved to be highly effective without pyrazinamide, offering a viable option for strains resistant to this drug.
Although the study’s scope was limited by the small quantities of the imageable antibiotics used, the results are promising. The researchers acknowledge that further clinical trials are necessary to confirm these findings and to evaluate the regimens’ safety and efficacy in broader populations.
For more detailed information, refer to the full study published in Nature Communications: Nature Communications Article.