Definitions:
The following definitions and terminology are used by WHO throughout its policy recommendations on COVID-19 vaccination. This note focuses only on booster doses.
- Booster doses are administered to a vaccinated population that has completed a primary vaccination series (currently one or two doses of EUL COVID-19 vaccine depending on the product) when, with time, the immunity and clinical protection has fallen below a rate deemed sufficient in that population. The objective of a booster dose is to restore vaccine effectiveness from that deemed no longer sufficient.
- Additional doses of a vaccine may be needed as part of an extended primary series for target populations where the immune response rate following the standard primary series is deemed insufficient. The objective of an additional dose in the primary series is to enhance the immune response to establish a sufficient level of effectiveness against disease. In particular, immunocompromised individuals often fail to mount a protective immune response after a standard primary series, but also older adults may respond poorly to a standard primary series with some vaccines (1).
Global context
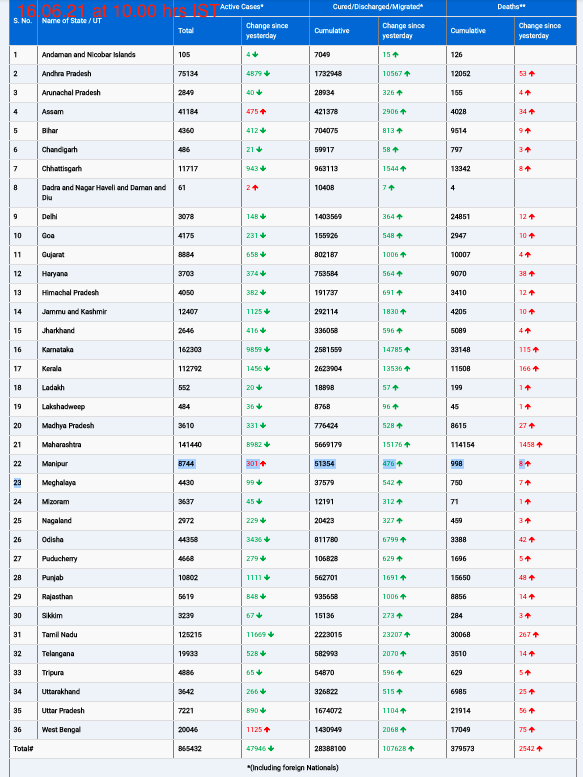
The Director-General of WHO has called for a moratorium on booster vaccination for healthy adults until the end of 2021 to counter the persisting and profound inequity in global vaccine access (2). While many countries are far from reaching the 40% coverage target by the end of 2021, other countries have vaccinated well beyond this threshold, already reaching children and implementing extensive booster vaccination programmes. At the time of the release of this statement, globally about 20% of COVID-19 vaccine doses, daily, are used for booster or additional dose vaccination.
Vaccine booster dose policy decisions should be based on evidence of individual and public health benefit and obligations to secure global equity in vaccine access as a means to minimize health impacts and transmission, and thereby reduce the risk of variants and prolongation of the pandemic. While vaccine supply is growing, it is not evenly distributed. Lower-income countries have had far less access, and face unpredictable and irregular supply. Within countries, equity considerations support improving coverage of the primary vaccination series in high-risk populations as the top priority use of vaccine doses (3).
Public health goals for the administration of booster doses
The WHO roadmap on the prioritization of vaccine use in situations of limited supply (hereafter: the Roadmap), (3) as well as the Strategy to Achieve Global COVID-19 Vaccination by mid-2022 (4), define a hierarchy of public health goals in accordance with progressively increasing control of the COVID-19 pandemic. Among those, the primary global goal for the acute phase of the pandemic is to reduce deaths and severe disease due to COVID-19 and to protect the health system. The level of population vaccination coverage needed to achieve this goal may differ between countries.
Subsequent public health goals include the reduction of COVID-19 disease burden and of viral transmission, to restore social and economic life, as described in WHO’s Strategy to Achieve Global COVID-19 Vaccination by mid-2022. These goals and vaccine use cases should be pursued only when priority risk groups have full access to vaccines in order to achieve the primary objective of substantial reduction in severe disease and mortality.
Evidence of waning protection from primary vaccination series
The vast majority of current infections and COVID-19 cases are observed in unvaccinated people. If breakthroughs occur in vaccinated persons, in most cases events are less severe than those in unvaccinated persons. However, emerging data consistently show a decline in vaccine effectiveness against SARS-CoV2 infection and COVID-19 with time since vaccination, and more significant decline in older adults. This evidence is mostly based on observational studies that may be subject to confounding factors (5).
Based on a recent systematic review and meta-regression analysis (6), across the four WHO EUL COVID-19 vaccines with the most data (i.e., BNT162b2, mRNA 1273, Ad26.COV2.S and ChAdOx1-S [recombinant] vaccine), vaccine effectiveness against severe COVID-19 decreased by about 8% (95% confidence interval (CI): 4-15%) over a period of 6 months in all age groups. In adults above 50 years, vaccine effectiveness against severe disease decreased by about 10% (95% CI: 6 – 15%) over the same period. Vaccine effectiveness against symptomatic disease decreased by 32% (95% CI: 11 – 69%) for those above 50 years of age.
For some inactivated vaccines (CoronaVac and COVID-19 vaccine BIBP), WHO has already issued the recommendation for the administration of an additional dose to those aged 60 years or older as part of the primary series to make initial immunity more robust (7, 8).
The degree of waning of immunity differs between vaccine products and target populations. Circulating viruses – in particular variants of concern; the extent of prior infection within a community at the time of primary vaccination; the primary vaccination schedule used (i.e. dose interval) and intensity of exposure are all likely to play a role in the findings on waning of protection but cannot be systematically assessed from current studies.
Evidence of booster vaccination performance
In several jurisdictions, booster vaccination has been authorized by regulatory authorities and added to the product labels of BNT162b2, mRNA 1273 and Ad26.COV2.S. In addition, for ChAdOx1-S [recombinant] and CoronaVac, COVID-19 vaccine BIBP, BBV152 and NVX-CoV2373 vaccines, clinical trial data of booster doses are available. All studies to date show a strong anamnestic immunological response achieving or improving upon the peak antibody levels following the primary immunization series, but with insufficient data and too little follow-up to assess the kinetics and duration of the response. Both homologous and heterologous booster regimens are immunologically effective(9).
Because no correlate of protection has yet been defined, it is not possible to predict with high confidence vaccine performance of these heterologous schedules based on the immune response. Vaccine effectiveness data for a booster dose are being published from an increasing number of countries, but remain limited in follow-up time. All studies demonstrate an improvement in protection against infection; milder disease; as well as severe disease and death (10-14) .
Safety and reactogenicity studies are based on small-scale clinical trials and post-licensure data with limited follow-up. Overall, they show a similar safety profile to that observed after the second dose in the primary series. Regulatory authorities and advisory bodies have thus assessed a favourable benefit risk ratio of booster vaccination at an individual level.
Factors to be considered when developing a booster vaccination policy
Current situation in countries
At least 126 countries worldwide have already issued recommendations on booster or additional vaccination and more than 120 have started programmatic implementation. The majority of these countries are classified as high-income, or upper middle-income. No low-income country has yet introduced a booster vaccination programme. The most commonly prioritized target populations for booster doses are older adults, health workers and immunocompromised individuals (in immunocompromised individuals the booster dose is considered as an additional primary series vaccination dose by WHO). The degree of primary vaccination coverage in the eligible adult population varies. In several of these countries which are administering booster doses the coverage rates for complete primary vaccination are below 30%.
Global equity and supply
In view of the continued supply uncertainties in global vaccine access and equity, individual country vaccine booster dose policy decisions need to balance the public health benefits to their population with support for global equity in vaccine access necessary to address the virus evolution and pandemic impact.
Of concern are broad-based booster programmes, including the booster vaccination of population sub-groups at lower risk of severe disease. Global supply is increasing significantly and is projected to be sufficient for vaccination of the entire adult population globally, and boosters of high risk populations (as defined in the roadmap, in particular older adults and immunocompromised persons), by the first quarter of 2022. However, projections show that only later in 2022 supply will be sufficient for extensive use of boosters in all adults, and beyond, should they be broadly needed.
Even as supply has continued to ramp up, hurdles in access and distribution have led to the prevailing inequities that can only be resolved by high coverage and supply and through countries’ commitment to global vaccine goals and targets, and to assisting other countries in need.
Public health use case and optimization of vaccine impact
In accordance with the Roadmap and WHO’s Strategy to Achieve Global COVID-19 Vaccination by mid-2022, the first priority of a vaccination programme is to reduce mortality and severe disease and to protect health systems. The most important measure to achieve this goal is to maximize coverage among those most likely to become seriously ill and those most likely to become infected especially those who are critical for health system functioning. In order to do this, primary series coverage and selective booster options must be weighed and prioritized carefully. This priority also contributes to socioeconomic recovery, as the severity of COVID-19 and its potential to overwhelm health systems constitute a primary rationale for public health and social measures that restrict social and economic activity. To use vaccines first for those at lower risk of severe disease before achieving high primary series coverage and sustained protection through selective booster doses for those most likely to become seriously ill will reduce the impact that could be secured with the ongoing limited vaccine supply, and runs counter to the National Equity and Equal Respect principles of the Values Framework (15).
These use case principles are also supported by mathematical modeling on the optimization of public health impact of a limited vaccine supply. This modeling shows that greater reductions in mortality may be achieved by administering booster doses to high-risk populations than using those same doses for primary immunization of lower risk populations. As supply increases and vaccination is expanded to lower priority age groups, trade-offs may need to be considered as to prioritizing booster vaccination to high-risk populations over expanding primary immunization coverage to younger populations. WHO is currently not recommending the general vaccination of children and adolescents as the burden of severe disease in these age groups is low and high coverage has not yet been achieved in all countries among those groups who are at highest risk of severe disease (16).
Further data needs for booster vaccination policies
The decision to recommend and implement a booster dose is complex and requires, beyond clinical and epidemiological data, a consideration of national strategic and programmatic priorities, and importantly an assessment of the prioritization of globally limited vaccine supply. In this context, priority should be given to the prevention of severe disease and sustaining health systems. Evidence is accumulating to inform global recommendations, which may be refined as additional data become available. Additional data needs can be grouped into the following categories:
1. Assessing the need for booster doses:
Refined data on epidemiology and burden of disease:
- Epidemiology of breakthrough cases, by disease severity, age, co-morbidity and risk groups, exposure, type of vaccine and time since vaccination, and in the context of variants of concern
Refined vaccine-specific data:
- Efficacy, effectiveness, duration of protection of vaccination in the context of circulating variants of concern.
- Supplementary evidence from immunological studies assessing binding and neutralizing antibodies over time, as well as biomarkers of cellular and durable humoral immunity.
2. Assessing the performance of booster doses:
- Data on duration of protection of homologous and heterologous boosters.
- Safety and reactogenicity of booster vaccination, including heterologous boosting from larger-scale studies.
- Impact of booster vaccination on transmission.
3. Additional considerations include:
- Optimal timing of booster doses, possibility for dose-sparing for booster doses (e.g. fractional doses), booster needs in previously infected individuals, programmatic feasibility and sustainability, community perception and demand as well as equity considerations.
- Refined modeling studies to guide strategies to optimize the impact of vaccination.
Conclusions
The focus of COVID-19 immunization efforts must remain on decreasing death and severe disease, and the protection of the health care system. Public health and social measures continue to be an essential component of the COVID-19 prevention strategy, especially in light of the Omicron variant. In the context of ongoing global vaccine supply constraints and inequities, broad-based administration of booster doses risks exacerbating vaccine access by driving up demand in countries with substantial vaccine coverage and diverting supply while priority populations in some countries, or in subnational settings, have not yet received a primary vaccination series.
Introducing booster doses should be firmly evidence-driven and targeted to the population groups at highest risk of serious disease and those necessary to protect the health system. To date, the evidence indicates a minimal to modest reduction of vaccine protection against severe disease over the 6 months after the primary series. Waning of effectiveness against all clinical disease and infection is more pronounced. Duration of protection against the Omicron variant may be altered and is under active investigation. Evidence on waning vaccine effectiveness, in particular a decline in protection against severe disease in high-risk populations, calls for the development of vaccination strategies optimized for prevention of severe disease, including the targeted use of booster vaccination.
More data will be needed to understand the potential impact of booster vaccination on the duration of protection against severe disease, but also against mild disease, infection, and transmission, particularly in the context of emerging variants. Over time, as vaccination programmes effectively protect populations from severe disease and death, the protection against milder disease and the reduction of transmission become important additional considerations.
SAGE has deliberated on the evidence for booster doses and the optimization of vaccination programmes during its Extraordinary SAGE meeting on 7 December 2021, which is reflected in this interim statement. SAGE will further discuss policies to optimize the use of vaccines including the consideration of booster vaccination at its forthcoming meeting on 19 January 2022.