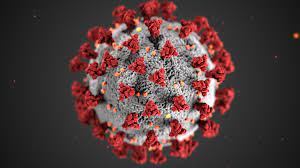
A recent study has revealed that despite stringent cleaning protocols, hospital sink drains continue to be a breeding ground for dangerous bacteria, contributing to the rise of healthcare-associated infections (HAIs). The findings underscore the global challenge of managing bacterial contamination in medical facilities.
HAIs primarily affect patients with weakened immune systems, often due to inadequate hygiene practices. These infections have become a major concern worldwide, accounting for approximately six percent of global hospital budgets, the study reported.
One of the key contributors to this issue is the widespread use of antibiotics, which can foster the development of antibiotic-resistant bacterial strains. When resistance genes are carried on mobile genetic elements, they can transfer between bacterial species, potentially leading to the emergence of new diseases.
“Here we show that hospital sink drains host bacterial populations that change over time, despite impeccable cleaning protocols in the particular hospital we looked at,” stated Dr. Margarita Gomila, a professor at the University of the Balearic Islands in Spain.
The study, published in Frontiers in Microbiology, highlights that controlling bacterial growth in drains and preventing colonization by new strains is a global challenge.
Findings from a Modern Hospital
The research focused on a modern university hospital in Majorca, built in 2001 and managed by the Balearic Islands’ health service. Despite routine cleaning with bleach, chemical disinfectants, pressurized steam every two weeks, and yearly hyperchlorination, the study identified a total of 67 different bacterial species in the hospital’s sink drains.
The highest bacterial diversity was found in general medicine and intensive care units, whereas the microbiology laboratory had the lowest. Newly opened intensive care units also exhibited significant bacterial diversity.
Among the most concerning bacteria identified were Stenotrophomonas species and Pseudomonas aeruginosa, both of which are known to cause ventilator-associated pneumonia and sepsis. Sixteen other Pseudomonas species, recognized by the World Health Organization (WHO) as major antibiotic resistance threats, were also detected, particularly in short-stay wards.
Other recurrent hospital-associated pathogens included Klebsiella pneumoniae in general medicine, Acinetobacter johnsonii and Acinetobacter ursingii in general medicine and intensive care, Enterobacter mori and Enterobacter quasiroggenkampii in short-stay wards, and Staphylococcus aureus in intensive care and hematology wards.
Addressing the Challenge
The researchers emphasized the critical need to understand the origin of these bacteria and their transmission pathways. Hospital drains, acting as reservoirs for both known and emerging pathogens, pose a significant challenge in infection control, especially given the rising antibiotic resistance among these microbes.
Efforts to mitigate these risks must go beyond routine cleaning, potentially incorporating innovative antimicrobial materials, frequent microbiological surveillance, and improved infection control strategies.
Disclaimer: This article is based on scientific research and aims to provide informational content. It does not serve as medical advice. Readers concerned about hospital-acquired infections should consult healthcare professionals for guidance on prevention and treatment measures.