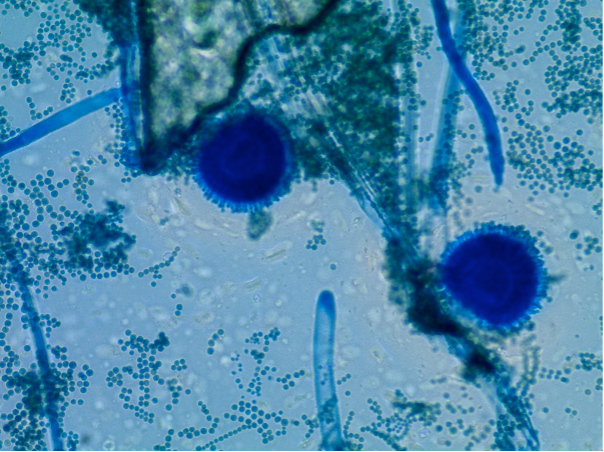
A groundbreaking study offers a glimmer of hope against mucormycosis, a devastating fungal infection often dubbed the “flesh-eating” fungus, which carries alarmingly high mortality rates, particularly among those with compromised immune systems. The infection, caused by Mucorales molds, has seen a surge in cases, especially during the COVID-19 pandemic, where it preyed on patients treated with high doses of corticosteroids, resulting in mortality rates nearing 60%.
Mucormycosis, endemic to regions like India, where it affects an estimated 200,000 people, also poses a significant threat in the United States, with approximately 4,000 cases reported annually. Unlike bacterial and viral infections, effective immunotherapies for this fungal disease have been notably absent.
However, research conducted by Ashraf Ibrahim, PhD, and Yiyou Gu, PhD, at The Lundquist Institute for Biomedical Innovation at Harbor-UCLA Medical Center, has yielded a potential breakthrough. Their study, published in Science Translational Medicine, details the development of a humanized monoclonal antibody, VX-01, that targets CotH, a crucial fungal cell surface protein responsible for the fungus’s ability to invade human cells and blood vessels.
“Mucormycosis is a devastating disease that usually occurs in patients who suffer from weakened immune system such as patients with poorly controlled diabetes, cancer patients undergoing chemotherapy, and transplant patients,” explained Ibrahim. The infection’s aggressive nature often necessitates drastic surgical interventions, including disfiguring procedures, to remove infected tissues.
The researchers found that VX-01 significantly enhances the efficacy of existing antifungal drug therapies by preventing the fungus from damaging blood vessels, thereby allowing the drugs to reach infected tissues more effectively. “Our humanized monoclonal antibody allows antifungal drug therapy to reach to infected tissues because it prevents fungal cells from damaging human cells and blood vessels,” Ibrahim said.
VX-01, a refined version of an earlier antibody, has demonstrated superior binding affinity to the fungus and reduced immunogenicity, making it safer and more effective for human use. Early tests have shown that VX-01 is safe, with no harmful effects on healthy cells, indicating its potential as a promising treatment for mucormycosis in vulnerable populations.
This development marks a significant step forward in combating a disease that has long challenged medical professionals, offering hope for improved treatment outcomes and reduced mortality rates.
Disclaimer: This article is based on information provided in the referenced study. Further research and clinical trials are necessary to confirm the efficacy and safety of VX-01 in treating mucormycosis in humans. The information provided here should not be interpreted as medical advice. Always consult with a healthcare professional for diagnosis and treatment of any medical condition.