Healthcare professionals are facing a growing concern as reports emerge of highly contagious and atypical fungal infections that are potentially misdiagnosed, posing significant public health risks. Recent studies have highlighted the emergence of sexually transmitted and drug-resistant strains of fungal infections, challenging conventional treatment methods and diagnostic practices.
The Nature of the Infections
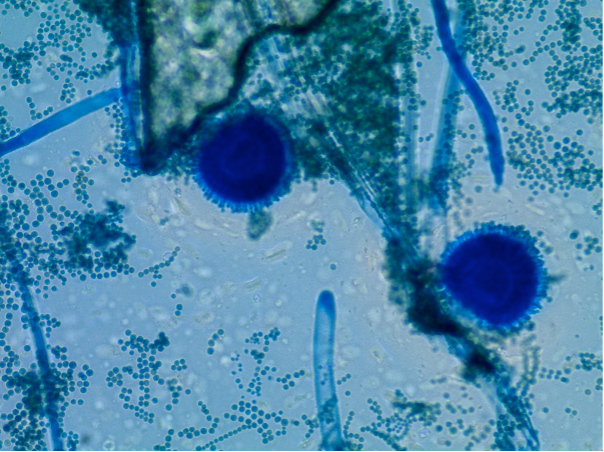
Two distinct fungal species, identified as Trichophyton mentagrophytes type VII (TMVII) and Trichophyton indotineae (T. indotineae), have recently gained attention for their unique characteristics and treatment challenges. TMVII, initially documented in Europe and now appearing in the United States, has been linked to cases of sexually transmitted infections, primarily affecting men who have sex with men. The infection, characterized by persistent and atypical rashes on the genitalia, buttocks, and limbs, can linger for months despite treatment with standard antifungal therapies like terbinafine.
In contrast, T. indotineae, prevalent in South Asia and now reported globally including in the U.S., exhibits resistance to terbinafine—a commonly prescribed antifungal medication. This resistance, attributed to genetic mutations that hinder drug effectiveness, complicates treatment regimens and necessitates alternative therapies like itraconazole, which come with their own set of challenges due to potential side effects and drug interactions.
Insights from Recent Studies
Recent research published in JAMA Dermatology has shed light on these fungal infections’ clinical presentations and challenges. Dr. Avrom Caplan and colleagues from NYU Langone Health emphasize the importance of heightened awareness among healthcare providers regarding the diagnostic complexities and treatment nuances associated with these emerging infections. The studies underscore the need for proactive screening, especially among sexually active individuals and those with recent travel histories to regions where these fungi are endemic.
Recommendations for Healthcare Providers
Healthcare providers are advised to maintain a high index of suspicion for fungal infections presenting with unusual rash patterns, particularly in regions susceptible to TMVII and T. indotineae. Direct inquiries about genital and skin symptoms are crucial, as patients may not spontaneously report these issues. Early detection and appropriate treatment tailored to the specific fungal strain are essential to mitigate the spread and impact of these infections.
Future Directions in Research
Dr. Caplan and his team plan to collaborate with international experts to further investigate these fungal strains’ epidemiology, resistance mechanisms, and optimal treatment strategies. This collaborative effort aims to enhance diagnostic capabilities and therapeutic outcomes, addressing the evolving challenges posed by emerging fungal infections in dermatological practice.
In conclusion, while the prevalence of TMVII and T. indotineae remains relatively low in the U.S. compared to endemic regions, vigilance among healthcare providers is crucial. By staying informed and proactive, healthcare professionals can effectively manage and contain these emerging fungal threats, safeguarding public health and improving patient outcomes.
This article summarizes the current understanding of emerging fungal infections based on recent studies and expert insights, highlighting the evolving landscape of dermatological challenges in healthcare today.